BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
URL: http://journal.zums.ac.ir/article-1-5949-en.html
2- Department of Otolaryngology, Hearing Disorders Research Center of Beasat Hospital, Hamadan University of Medical Sciences, Hamadan, Iran ,
✅ We present a case of THS in which the course of the disease suggested this idiopathic condition which occurred after wide mastoidectomy. The patient was diabetic and had a huge pituitary gland adenoma. Partial petrosectomy, laboratory tests, and imaging studies were normal. We named this condition ‘Tolosa-Hunt-Like Syndrome’.
The International Classification of Headache Disorders defines Tolosa-Hunt syndrome (THS) as an orbital pain that often occurs on one side. It may be associated with paresis of some cranial nerves. The etiology of this syndrome is unknown; however, some histopathological studies have shown granulomatous inflammation in the cavernous sinus, pituitary adenoma, or superior orbital fissure (1). This syndrome leads to painful ophthalmoplegia (PO), which usually has dangerous causes. Thus, the physician should be aware of other differential diagnoses such as diabetes, meningitis, vasculitis, sarcoidosis, and brain or orbital tumors when diagnosing the disease (2).
THS has been associated with other inflammatory diseases such as Sarcoidosis, Wegener’s granulomatosis, and systemic lupus erythematosus (SLE) (3).
The differential diagnoses of THS are broad and sometimes dangerous. Thus, early and appropriate imaging and laboratory investigations are critical for timely diagnosis and management of THS.
Cranial nerves located near the cavernous sinus, or superior orbital fissure such as oculomotor, trochlear, and/or abducens nerves, may be affected. Other cranial nerves, such as the maxillary (4) and mandibular branches of the trigeminal nerve and the facial nerve (5), could be involved in rare instances.
A patient with THS may experience nausea or vomiting. These may be due to severe pain, as they quickly resolve with pain relief treatments. Other systemic or neurological symptoms have not been reported. We present a case with all the characteristics of THS after radical mastoidectomy and petrosectomy. No reports of similar cases of THS after mastoidectomy were found in the literature.
A 44-year-old congenitally bilaterally deaf and diabetic woman was referred to the otolaryngology department of Besat University Hospital, Hamadan University of Medical Sciences, Iran, with a right postauricular abscess. She was a known case of pituitary gland adenoma with acromegaly (Figure 1). The pituitary gland adenoma was not operable because of carotid artery encasement. We hospitalized the patient to drain the abscess. Massive inflammation was observed in her right mastoid air cells via magnetic resonance imaging (MRI) (Figure 2).
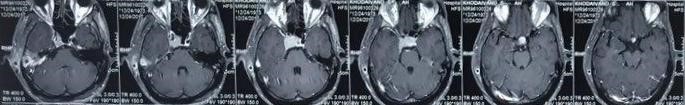
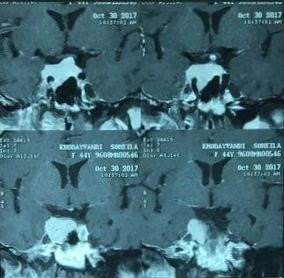
Figure 1. Brain T1 weighted MRI with contrast shows a huge pituitary gland adenoma with extension to the right cavernous sinus and internal carotid artery encasement.
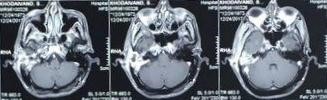
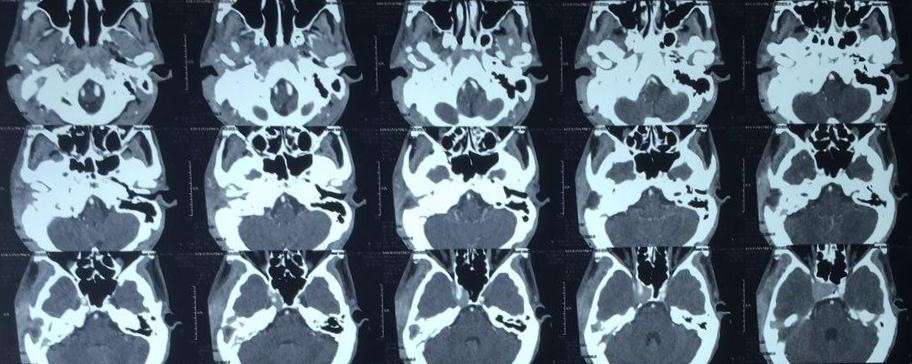
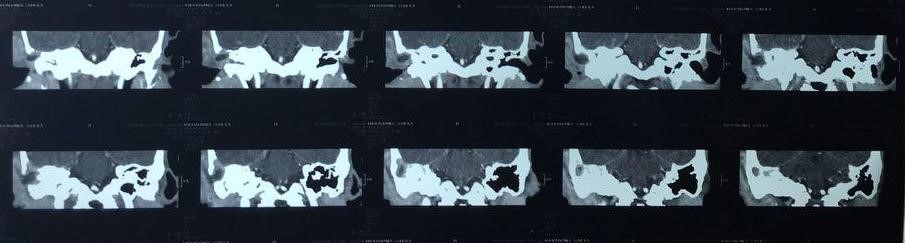
Figure 2. A) Temporal bone T1 weighted MRI with contrast and B) temporal bone CT scan shows right massive right mastoid inflammation.
After drainage of the right postauricular abscess and mastoidectomy, a partial petrosectomy was performed since the inflammation had expanded to the petrous apex. The involved tissues were removed from the middle ear and all mastoid air cells by preserving the facial nerve and labyrinth. Finally, radical mastoidectomy was done since the patient was congenitally bilaterally deaf.
After the surgery, the patient complained of a headache and severe deep right retro-orbital pain. Examinations, workups, and consultations with a neurologist, neurosurgeon, ophthalmologist, and endocrinologist revealed right pan ophthalmoplegia, ptosis, unreactive right pupil, decreased right visual acuity (20/200), a swollen optic disc in the right eye, and a normal optic disc in the left eye (Video 1). Sensation was decreased on the right side of the patient’s forehead and, thus, in the optic, oculomotor, trochlear nerves. The ophthalmic branch of the trigeminal nerve and abducens nerve were involved.
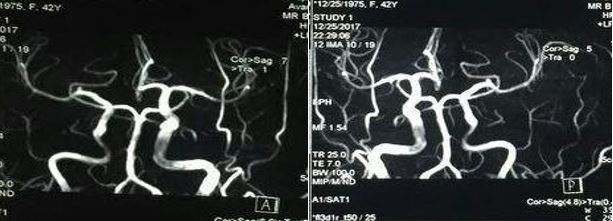
Consciousness level was appropriate (Glasgow Coma Scale=15). Blood glucose and other laboratory tests were normal. No changes were observed in the soft tissue or orbital fat in the MRI, and no changes were apparent in comparison with a previous study of adenoma. Lumbar puncture was not done because there was no doubt about the presence of an intracranial infection. Magnetic resonance angiography (MRA) and venography revealed normal blood flow in the internal carotid system and cavernous sinus (Figure 3).
After excluding other causes of PO, the diagnosis of THS was confirmed. Conservative treatment was performed. Ophthalmoplegia, ptosis, decreased visual acuity, unreactive pupils, and a swollen optic disc were resolved, one by one, after two weeks.
Figure 3. Brain Magnetic Resonance Angiography shows normal blood flow in internal carotid artery and cavernous sinus.
Discussion
Tolosa (6) and Hunt et al. (7) reported the first patient with THS in a related article. They defined THS based on the following clinical criteria: 1) paresis of the ophthalmic division of trigeminal nerve and/or paresis of the oculomotor, trochlear, and abducens nerves, with rare involvement of other cranial nerves such as the optic nerve or the sympathetic fibers along the cavernous sinus, 2) permanent retro-orbital pain, 3) symptoms lasting days or weeks, 4) suitable response to corticosteroid, 5) occasional spontaneous remission, and 6) recurrent attacks. Angiography and plain film should be used before computed tomography (CT) and MRI to exclude pituitary tumors, aneurysm, meningioma, or metastasis.
Schuknecht et al. conducted a study of 20 episodes of THS in 15 patients. Pathological tissue was observed around the ipsilateral cavernous carotid artery in all cases. Involvement of superior orbital fissure occurred in 13 (65%) of 20 episodes, and the extension of inflammation into the orbital apex was seen in eight (40%) of 20 episodes. In most cases, the cavernous sinus was affected (8). In our case, both the orbital apex and superior orbital fissure were affected according to the symptoms.
If anti-inflammatory drugs are started quickly, THS will have no side effects, but occasionally, it may lead to significant complications such as blindness due to optic nerve involvement. Thus, the physician should be aware of the clinical symptoms of all diseases that cause PO and think quickly to prevent further complications such as permanent blindness and ophthalmoplegia (9).
In a study by Youssem et al., there were low signal preserving fat, isointense to muscles (on short TR/TE MRI images), and abnormal soft tissue around the ipsilateral cavernous carotid artery in eight of nine cases (10). In our case, the intensity was normal in T1 and T2 weighted MRI.
Chronic nonspecific inflammatory changes have been reported in some studies. These changes can occur with or (sometimes) without granuloma around the cavernous carotid artery (7, 11). Drevelengas reported a case of a patient with THS that involved erosion of the sella. A CT scan also showed left cavernous sinus enlargement and a soft tissue mass in the sphenoid sinus (12). In our case, CT was normal, and no erosion was reported.
THS can occur at any age and has been equally reported in both sexes. The involvement of cranial nerves in THS is changeable. In a similar study, the oculomotor nerve (91%) and trochlear nerve (91%) were most commonly involved, while the abducens nerve was less often involved (68%) (13). In our case, the optic, oculomotor, trochlear, trigeminal, and abducens cranial nerves were involved.
In a systematic review, Curone et al. (14) examined the prevalence of cranial nerve involvement. The least involved nerve was the oculomotor nerve (39%), and the most involved nerve was the ophthalmic branch of the trigeminal nerve (83%). In our case, both nerves were involved.
Differential diagnoses of THS are very common (e.g. sarcoidosis, Wegener’s granulomatosis, aspergillosis, metastasis, brain tumors such as meningioma, brain lymphoma, ophthalmoplegic migraines, multiple sclerosis, and diabetic neuropathy). In summary, clinical examinations, imaging findings, and the exclusion of other differential diagnoses can help a physician diagnose THS. In our case, CT and MRI were normal, and we excluded all of differential diagnoses. A conservative treatment was performed. All symptoms related to the THS improved, one by one, after two weeks.
Conclusion
In this study, the patient was diabetic and congenitally bilaterally deaf. She had a huge pituitary gland adenoma, and her symptoms appeared after a wide mastoidectomy and partial petrosectomy. Therefore, we cannot state that this is a case of THS exactly. Thus, we think a more accurate name for this case is “Tolosa-Hunt-Like Syndrome.”
We recommend that ear surgeons should be aware of the nature of THS, which may have unusual manifestations after wide mastoidectomy-partial petrosectomy so that they can avoid unnecessary surgical procedures and medical interventions. Also, ear surgeons should be aware that this condition responds well to steroids.
Acknowledgements
The authors thank all those who helped them writing this article.
Ethical considerations
Ethical issues (Including plagiarism, informed consent, misconduct, data fabrication and/or falsification, double publication and/or submission, redundancy, etc.) have been completely observed by the authors.
Funding and support
This research resulted from an independent research without receiving any financial support.
Conflicts of Interest
Authors declared no conflict of interests.
Received: 2020/03/9 | Accepted: 2020/06/16 | Published: 2020/11/14
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |