BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
URL: http://journal.zums.ac.ir/article-1-5954-en.html
2- Cardiovascular Research Center, Shiraz University of Medical Sciences, Shiraz, Iran.
3- Dept. of Nursing, School of Nursing, Sabzevar University of Medical Sciences, Sabzevar, Iran ,
4- Heshmatie Hospital, Sabzevar University of Medical Sciences, Sabzevar, Iran.
✅ The repeated angiography indicated a good blood flow to the left upper distal limb. Minimally invasive methods, such as catheter-based thrombolytic therapy may be a suitable alternative for patients with viable limb acute ischemia.
The subclavian artery is located along the axillary artery. It provides various branches, including vertebral arteries that supply about 20% of brain blood (1). Axillary artery thrombosis is an occlusion in the axillary artery path accompanied by acute limb ischemia (ALI) symptoms in the upper limb causing significant ischemic symptoms. This condition may damage vital organs, including the brain or rarely heart. Therefore, axillary artery thrombosis is associated with a high risk of stroke and mortality (2).
Axillary artery thrombosis is a rare phenomenon that affects 3%-4% of the total population and accounts for approximately 11%-18% of peripheral artery disease cases (1). Atherosclerosis is the most prevalent facilitating etiology for thrombosis with less common causes being arthritis, radiation exposure, nerve compression syndrome, neurofibromatosis, and dysplasia (3). There are few studies about the successful treatment of axillary artery thrombosis by thrombolytic therapy thorough catheterization. Oliveira in 2014 presented a 45-year-old woman with left upper ALI with three days of progression after the distension of scapulohumeral articulation. Although digital amputation was finally performed, the hand was saved through thrombectomy and catheter-directed thrombolysis (4).
The ALI, as one of the results of arterial thrombosis, is a sudden decrease in limb perfusion posing a potential threat to limb survival. It may occur by involving any of the vessels, such as the axillary artery. The prevalence of this vascular accident is four times higher in the left subclavian artery, compared to the right subclavian artery (5).
Patients with subclavian artery thrombosis may refer to the emergency department (ED) with various or specific clinical symptoms known as six Ps (i.e., pain, poikilothermia, paresthesia, paralysis, pulselessness, and pallor) (6). Other symptoms of axillary artery thrombosis and ALI, typically in the upper limb, can include decreased arm movement, the loss of pulse, remarkable reduction in the blood pressure of the affected side, limb coldness, muscle weakness and fatigue, pain during rest, and finger necrosis. Neurological symptoms, including visual impairment, syncope, paresthesia, ataxia, dizziness, dysphasia, and dysarthria result from decreased blood flow to the vertebrobasilar arterial system (2).
Limb assessment determines whether the limb is viable, threatened, or irreversibly damaged. Rapid onset of symptoms can be helpful in the diagnosis of subclavian artery thrombosis; however, angiography is still the gold standard diagnostic method (7). Prompt revascularization by catheter-based thrombolysis or surgical reconstruction reduces the risk of limb loss. Catheter-directed thrombolysis is the preferred treatment for a viable or marginally threatened limb and recent occlusion. Amputation is performed in patients with irreversible damages (3). Thrombolytic agents are used intravenously or through catheter placement. It should be noted that bleeding is the most frequent complication at the catheter insertion site.
In the case of clinical suspicion, diagnostic tests and necessary therapeutic interventions should be performed. Therefore, timely treatment can save patients from certain death or permanent limb loss (8). Managing acute arterial obstruction is a challenge for vascular specialists. Surgical thrombo-embolectomy and bypass grafting have been known as the bases of treatment for many years (9). The present study describes a thrombolytic therapy procedure and presents a case of left subclavian artery thrombosis with acute clinical symptoms.
The present case report was approved by the Ethics Committee of Sabzevar University of Medical Sciences (ID IR.MEDSAB.REC.1399.102). The patient was an 82-year-old woman, who was referred to the ED of Heshmatie Hospital, Sabzevar, Iran. Patient symptoms included pain and reduced function of the left upper limb during previous hours. According to his caregivers, she had no history of illness or medication consumption, except blood hypertension and related medicines. Moreover, the patient experienced cardiac dysrhythmia (atrial fibrillation) one month ago. There was no history of smoking or opium consumption.
The vital signs of the individual were recorded as BP: 140/80, PR: 125, RR: 26, and T: 37.5 oral. The assessment was performed based on limb appearance, body temperature, pulse, muscular strength, and sensation. The left-arm blood pressure was not measurable at the time of admission to the ED. The left upper limb was cold in palpation with moderate paresthesia. Furthermore, radial, ulnar, and brachial pulses were undetectable in the left upper limb. Blood flow to extremities was evaluated using duplex ultrasound. Blood supply to the distal left upper limbs was found to be very poor.
Neurologic examination revealed normal muscular strength in the right side of the body, while it was 3.5 for the left upper extremity. In inspection, it was also pale, in comparison with the right upper limb. No obvious swelling was observed and the lower extremities pulse was full and symmetrical. The organs were normal in the initial physical examinations.
Laboratory findings showed normal values for hematology tests. On the other hand, high creatinine (2 mg/dL) and high cholesterol (280 mg/dL) levels were detected in serum biochemistry tests. In this patient, hypertension and high cholesterol were the leading causes of acute thrombosis and the formation of atherosclerotic plaque. The patient signed informed consent for participation in the current study.
Compromised left upper extremity blood flow was revealed in ultrasonography. A dilated echogenic thrombus had blocked the brachial artery lumen of the left upper limb and distal antecubital expanding to the axillary and left subclavian arteries. Conventional angiography with the lowest amount of contrast agent through the right femoral artery indicated an axillary artery thrombosis. The lack of blood flow was observed in the distal part of the thrombosis (Figure 1). Subclavian artery thrombosis detection and ALI diagnosis were confirmed following history evaluation and physical examination (six Ps).
Anticoagulant therapy was carried out by heparin. Considering the presence of thrombosis at the proximal area of the axillary artery and the distal subclavian artery, catheter-directed thrombolysis seemed the best treatment. A catheter with side holes was transmitted to the abdominal/thoracic aorta pathway through a femoral sheath and was directed to the subclavian artery. Afterwards, it was inserted into the arterial thrombus. The injection of alteplase as a thrombolytic medication through a catheter was started at the dose of 0.5 mg/h to overcome arterial pressure through the infusion pump. In addition, a low dose of heparin was infused intravenously.
Sixteen hours after treatment onset, the pain was significantly reduced, the left hand became warm, and a slight pulse was manifested. Moreover, the skin color became normal indicating an appropriate treatment response. Bleeding was well controlled at the catheter site. After 24 h, the contrast agent was injected by repeated angiography via the inserted catheter at the site to confirm the thrombosis-dissolution. The latter practice demonstrated a suitable blood flow to the left upper distal limb (Figure 2).
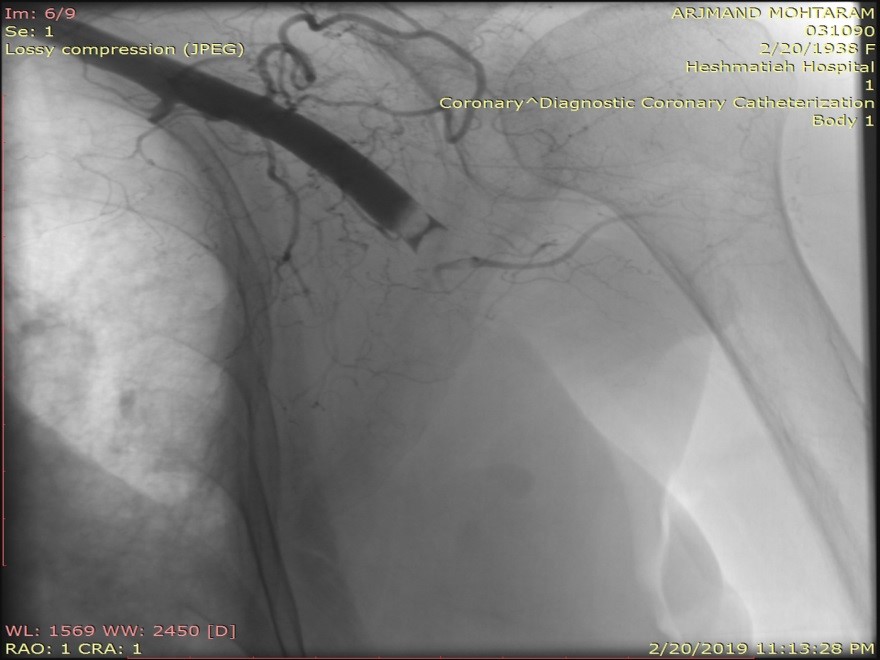
Figure1: The angiography picture before thrombolysis of the left axillary-subclavian artery thrombosis

Figure2: The angiography picture after thrombolysis of the left axillary-subclavian artery thrombosis
Discussion
Most of the times, subclavian thrombosis treatment requires aggressive procedures, such as open surgery and embolectomy (10). The majority of the patients with other underlying illnesses, including coronary artery disease, diabetes, and hypertension are at high risk for open surgery relevant complications. Consequently, nowadays, minimally invasive procedures are regarded as a better option for treating these patients. Currently, about 40% of damaged peripheral vascular patients are treated by interventional methods, namely stenting, ballooning, and mechanical thrombectomy (11).
One of the common therapies for patients with ALI is thromboembolectomy surgery using Fogarty arterial embolectomy catheter by a vascular surgeon. Another treatment is catheter-based thrombolysis by percutaneous transluminal angioplasty (12). The condition of patients determines which invasive therapy should be performed. Limb amputation is carried out in cases with complete gangrene (13).
Catheter-directed thrombolysis is one of the minimally invasive treatments for arterial occlusion. Ebben and colleagues (2019) conducted a retrospective review of patients who underwent catheter-directed thrombolysis for ALI during 2011-2016. The study outcomes showed that the angiographic potency and clinical success rates were more than 60% (8). Minimally invasive methods, such as catheter-based thrombolytic therapy could be more favorable alternatives. Alteplase is a preferable fibrinolytic and thrombolytic agent to the other fibrinolytic medications, namely streptokinase and reteplase (14).
In the present study, there were numerous surgical procedure hazards for the patient, including general anesthesia complications and cardiopulmonary risks concerning the age of the patient, atrial fibrillation rhythm, and high creatinine level. Therefore, the concurrent administration of anticoagulant and thrombolytic therapy was selected as the best treatment. Overall, minimally invasive methods may be a good alternative for invasive ones. Particularly, in the applied technique, the thrombosis was resolved through the administration of a thrombolytic agent during an angiography without anesthesia. Immediately after the procedure and arterial sheath removal, recovery was observed based on clinical signs and symptoms. Following repeated angiography, an apparent improvement was noted in the patient vascular status.
Conclusion
Catheter-based thrombolytic therapy is primarily reserved for patients with acute viable limb ischemia. As observed in the presented case, thrombolytic therapy is recommended to be considered as an alternative therapeutic method for patients with artery thrombosis due to the rapid response of the patient, shorter treatment time, and lower cost, compared to common and sometimes unsuccessful therapies.
Author disclosure statement
The authors have no financial interests related to the manuscript material.
Funding
The authors received no financial supports for the research of this article.
Conflicts of Interest
The authors declared no conflict of interest.
Received: 2020/03/22 | Accepted: 2020/12/16 | Published: 2021/02/28
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |