BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
URL: http://journal.zums.ac.ir/article-1-5975-en.html


 , Mohammad Reza Piran Aghl1
, Mohammad Reza Piran Aghl1 

 , Omran Ahmadi1
, Omran Ahmadi1 

 , Abdolhossein Pournajaf2
, Abdolhossein Pournajaf2 

 , Majid Seififard3
, Majid Seififard3 

 , Mehrdad Kazemi2
, Mehrdad Kazemi2 

 , Masoud Pournajaf4
, Masoud Pournajaf4 

 , Meghdad Kazemi *5
, Meghdad Kazemi *5 


2- Dept. of Occupational Health Engineering, School of Public Health, Ilam University of Medical Sciences, Ilam, Iran
3- Dept. of Nursing, Faculty of Nursing and Midwifery, Ilam University of Medical Sciences, Ilam, Iran
4- HSE Attendant of the Synthetic Cycle Power Plant of Nowshahr, Nowshahr, Iran
5- Dept. of Occupational Health Engineering, School of Public Health, Ilam University of Medical Sciences, Ilam, Iran ,
✅ Sleep problems and occupational fatigue in nurses of the female Post-CCU and nursing stations were higher and lower than the nurses working in the other hospital wards, respectively. Furthermore, the second job variable was found to be important and influential.
In recent years, sleep disorders and difficulties are increasing because of labor division and the expansion of a 24 h society (1). Sleep is one of the basic needs of humans and plays a significant role in recovery from fatigue and loss of power. Therefore, any disorder in natural sleep process not only brings about mental and somatic problems but also decreases the efficiency of the individual. Any disorder in the sleep cycle disrupts other physiological functions of the body. Sleep disorders lead to some difficulties, including diminished appetite, feeling exhausted, lack of concentration, intensification of illnesses, and somatic problems (2).
Various factors, such as insufficient sleep affect sleep quality. Sleep quality usually augments with deeper sleep and fewer dreams. Unsuitable sleep quality results in some side effects, including fatigue, health disorders (e.g., cardiac diseases, cancer, malignancies, blood hypertension, diabetes, enteric problems, depression, decreased libido, obesity, and higher mortality risk), cognitive performance disorders (e.g., learning, retention, consciousness, concentration, and reasoning), occupational events, irritability, and improper decision-making. (3).
In a study by Itani et al. on Japanese population, 14.6% of women and 12.2% of men had symptoms of insomnia. Moreover, 4.2% and 3.2% of women and men reported daytime disorders, respectively (4). Kim et al. indicated that a higher proportion of workers complained of insomnia than other people (5).
Nowadays, fatigue is one of the prevalent problems among all individuals and has transformed into an inseparable part of their life (6). The complexity of fatigue and the diversity of its components prevent the researchers from assigning it to a comprehensive definition. However, in the simplest condition, fatigue can be defined as a feeling of disability and weakness that reduces the capacity of individuals to do their job and daily activities leading to diminished performance. Occupational fatigue has various effects, namely a decline in job performance and satisfaction along with cardiovascular, mental, and musculoskeletal disorders, and injuries associated with their job (e.g., needle stick and human errors in the drug delivery process to the patient) (6, 7).
According to Winwood et al., occupational fatigue falls into the three categories of acute, chronic, and inter-shift recovery (IR). Acute fatigue (AF) is a condition in which an individual's energy is depleted due to working to the extent of not being able to carry out ordinary responsibilities during non-working hours (8). The AF is known to be transient and obviated by resting. Chronic fatigue (CF) results from the continuation of AF or the inability to eliminate AF. The CF develops from long-term incompatibility with stress or work and involves a combination of mental, physical, and emotional components (9).
The progression of fatigue from acute to chronic can be due to the insufficient IR of fatigue. Insufficient recovery from occupational fatigue leads to reduced efficiency, health problems, patients leaving the hospital, anxiety, and deciding to quit job. Sufficient and appropriate recovery from fatigue in the workplace results in the proper accountability of personnel for the patients and clients.
To prevent fatigue and its consequences, one needs to be aware of the reasons for fatigue and its side effects (8). The causes of fatigue are divided into the four following categories: 1) medical problems, such as diabetes, cardiovascular diseases, and thyroidal disorders, 2) lifestyle problems, including insomnia, alcohol and drug consumption, unsuitable diet, and personal factors, 3) work environment factors, namely working shift, unsuitable working pattern, unusual and long-term working hours, stressful workplace, individual and non-interactive working, and work overload, and 4) emotional problems, such as depression, anxiety, apprehension, sorrow, and grief (10).
In order to discover the relationship between fatigue and sleep disorders, a study was conducted on 5720 male and female working individuals. The results revealed that sleep disorder is the main predictive factor for CF in the working population (6). Abbassinia explained that shift work and resultant sleep disorders elevate the rate of fatigue (11).
Nurses are at risk for a high level of fatigue, improper sleep quality, implausible expectations, irregular and excessive working shifts, and innately tense working environments. According to the findings of different studies, more than half of the nurses have severe sleep problems, which can affect the quality of care provided by them (12). The results of a study by Ten Hoeve et al. on novice nurses revealed that 17.5% of nurses resigned from their jobs in the first year (13). In Iran, 80% of the working individuals comprise the healthcare system of country and provide healthcare services at the forefront.
Considering the aforementioned issues and the fact that the health of nurses can impose impact on the quality of the care they provide and patients’ health, nurses themselves should be healthy to be able to reach their ideal conditions and demonstrate desirable performance in the workplace (12). Consequently, the current study aimed to determine the level of occupational fatigue and sleep quality among nurses working in various wards of public hospitals.
This cross-sectional study was conducted during two months on 234 nurses working in various wards of Imam Khomeini and Mostafa Khomeini hospitals affiliated to Ilam University of Medical Sciences, Iran. Samples were selected using the convenience sampling method. The study population included the nurses of general admission, nursing station, Emergency, Pediatrics, Male and Female Surgical Units, Male and Female Internal Units, Neurology and Psychiatry, Intensive Care Unit (ICU), Neonatal Intensive Care Unit (NICU), Cardiac Care Unit (CCU), and Male and Female Post-CCU. The inclusion criteria entailed complete consent to participate in the study, not having any physical or mental disorders, and employment as a nurse with a work experience of at least six months in public hospitals affiliated to Ilam University of Medical Sciences. Data were collected using the demographic questionnaire, Occupational Fatigue Exhaustion Recovery (OFER15) scale (14), and the Pittsburgh Sleep Quality Index (PSQI) (15).
The present study was approved by the Ethics Committee of Ilam University of Medical Sciences with the ethics code of IR.MEDILAM.REC.1397.008. Ethical basics, such as explaining the purposes of the study, obtaining informed consent, protecting anonymity, data confidentiality, right to refuse participation in the study, and respecting the rights of the researchers were considered in the current study.
The OFER questionnaire was designed by Winwood et al. (8) and was localized in Iran by Javadpour et al. (14). The OFER includes 15 questions and consist of three subscales, namely CF-5, AF-5, and IR-5. Occupational fatigue (total score) and each of its subscales are divided into the three levels of low fatigue (high recovery), moderate fatigue (moderate recovery), and high fatigue (low recovery).
Each item is scored based on a seven-point Likert scale from 0 (strongly disagree) to 6 (strongly agree). In this questionnaire, a high score in AF, CF, and total fatigue indicates the high severity of fatigue, while a high IR score shows the low severity of recovery (10, 14). The most important benefits of this questionnaire include a high ability to measure fatigue in various jobs, such as nursing and distinguishing between AF and CF. In addition, this questionnaire has a specific IR subscale, while other surveys concerning occupational fatigue do not have IR subscale (10, 14).
The PSQI was designed by Buysse et al. (15), and the validity and reliability of this questionnaire have been confirmed in several studies (6, 16). The PSQI consists of 18 items and seven subscales, including daytime dysfunction, sleep disturbances, sleep latency, sleep efficiency, sleep duration, use of sleeping medications, and subjective sleep quality (15).
The latter questionnaire was completed in 5 min or less and inquired about the views of nurses regarding sleep quality during the previous month (15). Each PSQI subscale score and total score had the ranges of 0-3 and 0-21, respectively. A total score of 0-5 indicates "good sleep quality", a total score of 6-10 represents "relatively poor sleep quality", and a total score of 11-21 shows "poor sleep quality". Therefore, a total score of 6 ≤ reflects unsuitable sleep quality (6, 15, 16). Participants filled out questionnaires following providing the required information and instructions by the researchers.
The data were analyzed using the SPSS software version 21. The differences between the demographic and dependent variables (e.g., occupational fatigue and sleep quality) were analyzed by the independent t-test. Sleep quality and occupational fatigue in the nurses of different hospital wards were assessed utilizing the one-way analysis of variance (ANOVA). Moreover, mean and standard deviation were used to describe the numerical variables. The categorical variables were described by frequency and percentage. P-value < 0.05 was considered statistically significant.
In this study, out of 234 participating nurses, 102 were male and 132 were female. The ranges of the age and work experience of the subjects were 21-58 and 1-29 years, respectively. More than half of the nurses (54.7%) were married and 45.3% were single. The demographic characteristics and job data are shown in Tables 1 and 2..
Table 1. Demographic characteristics of participants
| Frequency (%) | Variables |
| Number of children | |
| 138 (59) | Zero |
| 39 (16.7) | One |
| 33 (14.1) | Two |
| 19 (8.1) | Three |
| 5 (2.1) | Four and more |
|
|
|
| 14 (6) | Yes |
| 220 (94) | No |
| Having a specific disease | |
| 8 (3.4) | Yes |
| 226 (96.6) | No |
| Income level | |
| 66 (28.2) | Proper salary |
| 168 (71.8) | Insufficient salary |
| Second job (in addition to the nursing job) | |
| 11 (4.7) | Yes |
| 223 (95.3) | No |
Table 2. Nurses working in various wards of hospitals
| Total | Mostafa Khomeini Hospital | Imam Khomeini Hospital | Hospital wards |
| Frequency (%) | Frequency (%) | Frequency (%) | |
| 40 (17.1) | 25 (18.1) | 15 (15.6) | Emergency |
| 11 (4.7) | 5 (3.6) | 6 (6.3) | General admission |
| 9 (3.8) | 0 | 9 (9.4) | Pediatrics |
| 12 (5.1) | 4 (2.9) | 8 (8.3) | Nursing station |
| 12 (5.1) | 8 (5.8) | 4 (4.2) | NICU |
| 16 (6.8) | 2 (1.4) | 14 (14.6) | Female surgical ward |
| 22 (9.4) | 0 | 22 (22.9) | Male surgical ward |
| 23 (9.8) | 5 (3.6) | 18 (18.8) | ICU |
| 13 (5.6) | 13 (9.4) | 0 | Male internal ward |
| 9 (3.8) | 9 (6.5) | 0 | Female internal ward |
| 8 (3.4) | 8 (5.8) | 0 | Male post-CCU |
| 8 (3.4) | 8 (5.8) | 0 | Female post-CCU |
| 34 (14.5) | 34 (24.6) | 0 | CCU |
| 17 (7.3) | 17 (12.3) | 0 | Neurology and psychiatry |
| 234 (100) | 138 (100) | 96 (100) | Total |
According to Table 1, in terms of the number of children, the highest and lowest frequencies belonged to the groups without children (59%) and with four children and more (2.1%), respectively. More than 90% of the study population were non-smokers and less than 5% had a specific disease and a second job. According to Table 2, the highest percentage of the nurses participating in the study was the nurses working in the Emergency (17.1%).
Based on the results of the one-way ANOVA test, the mean score of daytime dysfunction subscale was significantly different between the nurses of hospital wards (P<0.05). Our findings demonstrated that the highest and lowest scores of daytime dysfunction were for the nurses working in the Female Post-CCU (4.12±1.72) and nursing station (0.83±0.93), respectively. Comparison of sleep quality subscales among nurses working in various wards are summarized in Table 3.
According to the results of the one-way ANOVA test, a significant difference was observed between the hospital wards in terms of the mean scores of AF, CF, and total occupational fatigue (P<0.05). As indicated in Table 4, the highest and lowest scores of occupational fatigue were for the nurses working in Female Post-CCU (58.12±12.24) and nursing station (36.08±12.74), respectively. Comparison of occupational fatigue subscales between nurses working in diverse wards is shown in Table 4.
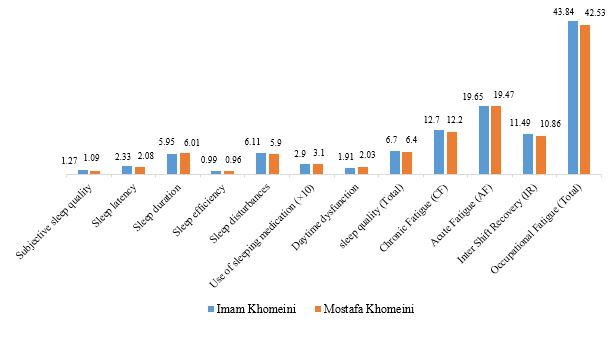
The findings of t-test did not show a significant difference between the mean scores of any subscales of sleep quality, occupational fatigue, and the hospital at which the nurses worked (P>0.05). However, the mean sleep quality (total) and occupational fatigue (total) in nurses working at Imam Khomeini Hospital were higher than those of the nurses working at Mostafa Khomeini Hospital. The results are shown in Figure 1.
The t-test indicated a significant difference between the mean scores of sleep latency, use of sleeping medications, AF subscales, and a second job (P<0.05) as the mean of all three subscales was higher in the nurses with a single job than the ones with a second job. Moreover, this test indicated a significant difference between the mean scores of sleep latency, sleep disturbance subscales, and income level (P<0.05) (Table 5).
Table 3. Mean score of sleep quality subscales in various wards
| Sleep quality subscales | Hospital wards | |||||||
|---|---|---|---|---|---|---|---|---|
| Sleep quality (total) | Daytime dysfunction | Use of sleeping medication | Sleep disturbances | Sleep efficiency | Sleep duration | Sleep latency | Subjective sleep quality | |
| Mean±SD | Mean±SD | Mean±SD | Mean±SD | Mean±SD | Mean±SD | Mean±SD | Mean±SD | |
| 6.22±2.69 | 1.7±1.36 | 0.32±0.61 | 6.37±3.8 | 0.98±0.16 | 5.98±1.37 | 1.95±1.75 | 1.15±0.76 | Emergency |
| 7.09±4.59 | 1.18±1.32 | 0.18±0.6 | 3.9±4.03 | 1±0.18 | 4.9±1.51 | 2.9±2.21 | 1.36±1.02 | General admission |
| 7.66±3.93 | 2.88±2.47 | 0.22±0.44 | 8.11±4.56 | 0.91±0.08 | 5.73±1.32 | 2.55±1.87 | 1.55±0.72 | Pediatrics |
| 3.83±2.32 | 0.83±0.93 | 0.0±0.0 | 3.91±3.89 | 0.95±0.08 | 6.27±1.19 | 1.16±1.33 | 0.58±0.51 | Nursing station |
| 6.25±4.39 | 2.16±2.12 | 0.41±0.99 | 4±2.79 | 1.01±0.17 | 6.52±1.5 | 1.75±1.54 | 1.33±0.98 | NICU |
| 7.06±4.04 | 2.37±1.85 | 0.43±0.81 | 6±5.22 | 0.96±0.16 | 5.93±1.48 | 2.31±1.95 | 1.18±0.83 | Female surgical ward |
| 6.13±2.47 | 1.5±1.14 | 0.22±0.42 | 5.18±4.73 | 1.05±0.4 | 6.19±1.13 | 2.18±1.43 | 1.18±0.58 | Male surgical ward |
| 7.6±4.27 | 2.13±1.74 | 0.47±0.79 | 7.43±4.6 | 0.95±0.25 | 5.82±1.77 | 2.65±2.01 | 1.26±0.96 | ICU |
| 8.53±4.59 | 2.92±1.75 | 0.3±0.63 | 6.07±3.9 | 0.91±0.17 | 5.66±2.31 | 3.07±2.13 | 1.53±1.12 | Male internal ward |
| 5.77±3.11 | 1.55±1.58 | 0.11±0.33 | 5.11±4.04 | 0.94±0.11 | 6.22±1.39 | 2.44±2.4 | 0.88±0.6 | Female internal ward |
| 7±2.92 | 2.37±2.55 | 0.25±0.7 | 4.62±4.43 | 0.89±0.09 | 5.95±1.65 | 3.12±1.72 | 1.12±0.64 | Male post-CCU |
| 8.37±3.37 | 4.12±1.72 | 0.25±0.46 | 7.62±6.94 | 1.01±0.13 | 5.5±1.51 | 2.75±2.18 | 1.12±0.35 | Female post-CCU |
| 5.97±3 | 2.05±1.77 | 0.26±0.51 | 5.88±4.53 | 0.95±0.15 | 6.15±1.43 | 1.61±1.07 | 1.08±0.62 | CCU |
| 6.05±3.96 | 1.58±2.18 | 0.47±1 | 7.76±6.31 | 0.95±0.09 | 6.27±1.51 | 1.94±1.34 | 1.05±0.65 | Neurology and psychiatry |
| 6.54±3.54 | 1.98±1.78 | 0.3±0.64 | 5.99±4.61 | 0.97±0.19 | 5.98±1.5 | 2.18±1.75 | 1.16±0.77 | Total |
| 0.108 | 0.003* | 0.824 | 0.216 | 0.757 | 0.593 | 0.088 | 0.275 | P-value |
Table 4. Mean score of occupational fatigue subscales in various wards
| Occupational fatigue subscales | Hospital wards | |||||||
|---|---|---|---|---|---|---|---|---|
| Occupational fatigue (total) | Inter-shift recovery (IR) | Acute fatigue (AF) | Chronic fatigue (CF) | |||||
| Mean±SD | Mean±SD | Mean±SD | Mean±SD | |||||
| 41.35±9.9 | 10.97±4.17 | 17.52±7.21 | 12.85±5.02 | Emergency | ||||
| 39.45±12.45 | 11.36±4.05 | 17.36±7.28 | 10.72±2.96 | General admission | ||||
| 47±14.54 | 10.44±4.27 | 22.66±9.52 | 13.88±5.27 | Pediatrics | ||||
| 36.08±12.74 | 9.83±3.37 | 15.75±7.05 | 10.5±4.64 | Nursing station | ||||
| 46.16±13.18 | 13.41±5.31 | 21.75±6.57 | 11±5.84 | NICU | ||||
| 46.5±13.34 | 11.87±4.47 | 21.75±7.79 | 12.87±5.18 | Female surgical ward | ||||
| 45.13±11.62 | 12±4.73 | 20.59±7.21 | 12.54±5.02 | Male surgical ward | ||||
| 45.56±13.13 | 11.26±5.12 | 20.52±7.79 | 13.78±5.27 | ICU | ||||
| 53.84 ± 21.1 | 11.23 ± 4.86 | 24.69 ± 9.66 | 17.92 ± 8.17 | Male internal ward | ||||
| 41.22±19.07 | 10.55±3.81 | 20.55±10.6 | 10.11±6.77 | Female internal ward | ||||
| 38.37±12.42 | 10±4.14 | 16.62±7.63 | 11.75±6.25 | Male post-CCU | ||||
| 58.12±12.24 | 13.5±6 | 27.62±7.81 | 17±5.09 | Female post-CCU | ||||
| 38.35 ± 11.37 | 10.7 ± 5.39 | 16.76 ± 7.13 | 10.88 ± 5.79 | CCU | ||||
| 38.11±15.27 | 9.35±3.12 | 19±8.26 | 9.76±7.35 | Neurology and psychiatry | ||||
| 43.06±13.84 | 11.11±4.58 | 19.53±8.05 | 12.41±5.87 | Total | ||||
| 0.001* | 0.613 | 0.005* | 0.006* | P-value | ||||
Table 5. .Comparing sleep quality and occupational fatigue subscales based on the number of jobs and income level
| Subscales | Number of jobs | Income level | ||||
| Single job | Second job | P-value |
Proper salary | Insufficient salary | P-value |
|
| Mean±SD | Mean±SD | Mean±SD | Mean±SD | |||
| Subjective sleep quality | 1.184±0.77 | 0.81±0.87 | 0.201 | 1.03±0.8 | 1.22±0.76 | 0.092 |
| Sleep latency | 2.238±1.75 | 1.09±1.37 | 0.034* | 1.72±1.8 | 2.34±1.7 | 0.016* |
| Sleep duration | 6.01±1.5 | 5.45±1.44 | 0.236 | 5.84±1.44 | 6.04±1.52 | 0.373 |
| Sleep efficiency | 0.97±0.19 | 1.01±0.2 | 0.47 | 1.01±0.28 | 0.95±0.15 | 0.064 |
| Sleep disturbances | 6.1±4.63 | 3.63±3.5 | 0.083 | 4.82±2.5 | 6.36±3.2 | 0.024* |
| Use of sleeping medication | 0.10±0.01 | 0.31±0.09 | 0.03* | 0.22±0.57 | 0.33±0.67 | 0.229 |
| Daytime dysfunction | 2±1.77 | 1.63±2.11 | 0.511 | 1.9±1 | 2.01±1.07 | 0.693 |
| Sleep quality (total) | 6.6±3.54 | 4.9±3.3 | 0.117 | 5.83±3.6 | 6.83±3.5 | 0.053 |
| Chronic fatigue (CF) | 12.5±5.9 | 10.63±5.14 | 0.306 | 11.63±6.07 | 12.71±5.78 | 0.207 |
| Acute fatigue (AF) | 19.8±7.95 | 14.09±8.6 | 0.021* | 18.93±8.18 | 19.77±8.01 | 0.477 |
| Inter-shift recovery (IR) | 11.07±4.46 | 12±7.05 | 0.676 | 11.9±4.9 | 10.8±4.42 | 0.099 |
| Occupational fatigue (total) | 43.38±13.82 | 36.72±13.4 | 0.12 | 42.48±14.94 | 43.3±13.43 | 0.687 |
Results of the t-test revealed that the smoking and non-smoking groups were significantly different in terms of the mean scores of sleep latency subscale (P<0.05) as the mean score of this subscale was higher in smokers than non-smokers. Furthermore, based on the results of this test, there was a significant difference between the diseased and healthy participants in terms of the mean scores of sleep disturbance subscale (P<0.05) as the mean score of this subscale was higher in diseased nurses than the healthy individuals.
Figure 1. Comparing sleep quality and occupational fatigue subscales between the two hospitals
Discussion
Fatigue in workplaces, especially in the workplace of nurses, has harmful effects on people performance and health. Poor and unsuitable sleep quality is recognized as one of the most important causes of fatigue. In the present study, occupational fatigue and sleep quality in the nurses working in different units of hospitals were investigated.
According to our results, the mean sleep quality in nurses of all the studied wards (except the nursing station) was unsuitable. Moreover, a significant difference was observed between the mean scores of daytime dysfunction subscale in distinct hospital wards. Ahmadabadi et al. compared the sleep quality of the nurses working in diverse hospital units at Imam Reza Hospital, Mashhad, Iran. Their results revealed that 100% of the nurses in the Burn Unit and 96% of the nurses in other wards had sleep problems (17), which was in agreement with the findings of the present study.
Rocha et al. reported a significant relationship between job stress and sleep quality in the nurses of a hospital. The results of the latter investigation demonstrated that the mean sleep quality was unsuitable in the nurses of different wards of the studied hospital (18). According to the literature and our results, nurses generally have sleep problems. In the current study, it seemed that factors, such as low stress levels, reduced workload, and the lack of patient care tasks led to proper sleep quality in nurses working in the nursing station.
Results of the present study revealed that the mean CF and IR subscales for all the nurses in different wards, as well as the mean AF and occupational fatigue (total) for all the nurses except the ones working in the Female Post-CCU were at a moderate level. Moreover, the hospital wards were significantly different in terms of the mean scores of CF, AF, and occupational fatigue (total) as the means of these subscales were higher in the Female Post-CCU than other units.
Post-CCU admits more patients than other ICUs. Therefore, nurses working in this unit had higher fatigue scores than the nurses in the other wards due to excessive mortality (compared to the other units), short and temporary hospitalization, and the unreasonable expectations of patients relative to the length of their hospital stay. In addition to the aforementioned reasons, the number of nurses working in this ward was low in the present study, which might be considered as the most important factor for managerial burnout (19) leading to more workload and fatigue. Furthermore, women experience more fatigue as a result of usually being weaker than men, performing housework, cooking, child caring, and having short rest time (20).
A review of the literature indicated that our results were not consistent with the findings of Abdul Rahman et al. (21) and Yoder et al. (22). Abdul Rahman et al. revealed that the most problematic AF, CF, and IR subscales belonged to nurses working in the Emergency (21). The major difference between the latter study and the present investigation was the number of wards in the study and the countries in which the studies were conducted (21). The present study was carried out in 14 units, while the study population in the study performed by Abdul Rahman et al. included the nurses of Emergency and ICU (21).
The discrepancy between the results of the current study and the investigation by Yoder et al. could be attributed to the study wards, sample size, country, and the questionnaires used to measure fatigue (22). It can be concluded from the findings of the present investigation and similar studies that despite the difference in the nature of nurses' work in different units, nursing occupation is regarded as a fatiguing job.
Our analysis showed a significant difference between diverse groups of the second job variable in terms of the mean of sleep latency, use of sleeping medications, and AF. Nurses with a second job seemed to have better sleep quality because of being away from the stressful hospital environment (compared to nurses with a single job), the lack of work uniformity, and the variability in work environment. In addition, these nurses had more residual energy (less depleted energy) at the end of working hours and felt fresher at the beginning of the next day due to shorter time spent at hospital, doing other jobs, and other factors mentioned earlier. Therefore, these nurses were found to have lower AF.
The study by Razmpa et al. aimed to determine sleep disorders and related effective factors among nurses. Their results did not show a significant relationship between having a second job and sleep disorders (23). The main reasons for the controversial results of the present study and the mentioned investigation were study population and the questionnaires used to assess sleep quality and disorders. In the study by Razmpa et al., the study population entailed nurses employed at Imam Khomeini Hospital affiliated to Tehran University of Medical Sciences. Moreover, these authors used the Sleep Impairment Index (SII) and Epworth Sleepiness Index (ESS) to assess sleep quality and disorders (23).
We found a significant difference between the means of sleep latency and sleep disturbances in different income levels as the mean score of both subscales in participants with appropriate salaries was lower than individuals with low salaries. Properly-paid nurses have better sleep quality than poorly-paid nurses because of their better financial condition, fewer financial problems, lower mental distress, and feeling more relaxed.
Results of the study completed by Ansari et al. on nurses working in the hospitals affiliated to Zahedan University of Medical Sciences, Iran, showed a statistically significant relationship between income and sleep patterns (24), which is in line with the results of the present study.
Kunzweiler et al. evaluated the level of sleep quality and influential factors among nurses. Their results revealed no significant relationship between income level and sleep quality (25), which was not in agreement with the results of the present study. The most important reasons for this discrepancy in results were study country, sample size, the gender of the participants, and the questionnaires used to assess sleep quality. In the study by Kunzweiler et al. on female nurses, the sample size was approximately two-third of the present study. In addition, a visual analogue scale (VAS) was utilized to measure sleep quality (25).
According to the results of the current study, the mean sleep latency was significantly different between the smokers and non-smokers as the mean of this variable was higher in smokers than non-smokers. Cigarette smoking augments the activity of reticular activating system (RAS) stimulating the body and eventually impairing sleep quality (26). Results of the present investigation were consistent with the studies by Tarhan et al. (16) and Yilmaz et al. (27).
We found a significant difference between the sleep disturbances of healthy and diseased participants as the mean of this variable was higher in diseased nurses than healthy nurses. It is expected that some factors, including pain, physical complaints, concerns about disease treatment (mental disease), and providing financial resources can cause sleep disturbances in diseased nurses. It should be noted that the type and nature of the disease affect sleep disturbances and these disturbances are considered as the symptoms of disease in a number of diseases, such as respiratory diseases, metabolic disorders, and urinary tract infections (28). Findings of the present study were consistent with the study by Adib-Hajbaghery et al. conducted on nurses working in Kashan Hospital, Iran (29). However, our results were not in line with the study conducted by Tarhan et al. aimed to evaluate sleep quality and its related factors in nurses working at a hospital in Istanbul, Turkey (16). These controversial results might be due to small sample size in the study performed by Tarhan et al.
Conclusion
According to the results of the present study, the rate of problems in the sleep quality and occupational fatigue of nurses working in the Female Post-CCU and nursing station were higher and lower than the nurses working in other hospital units, respectively. Moreover, the nurses working in hospital environment regardless of the hospital units are at a higher risk of having unsuitable sleep quality and high occupational fatigue. Sleep quality affects occupational fatigue and sleep quality conditions in nurses are more unfavorable than occupational fatigue. Therefore, the control of sleep quality is of higher priority than controlling occupational fatigue.
In the present study, out of the factors effective in sleep quality and occupational fatigue, having a second job in addition to nursing was recognized as an important factor. In conclusion, to improve sleep quality and diminish job-related fatigue, the authors recommend the following steps: teaching the importance and necessity of good sleep quality and the undesirable effects of poor sleep quality and occupational fatigue on the individuals’ health, teaching the skills that elevate resiliency, raising awareness about the important influences of smoking and how to quit smoking, employing new nurses in all hospital wards, especially the Female Post-CCU, prioritizing the selection of non-smokers, employing highly resilient individuals, giving a suitable salary to nurses, allocating certain places in the hospital environment for smoking, encouraging exercise, and creating variety in the workplace.
Acknowledgements
The present study was the result of a research project with grant no. 974003.16 which was funded by Honorable Deputy of Research and Technology of Ilam University of Medical Sciences. The authors would like to thank all the personnel and nurses of Imam Khomeini and Mostafa Khomeini Hospitals in Ilam city who participated in the survey and filled out the questionnaire.
Ethical considerations
Ethical issues (Including plagiarism, informed consent, misconduct, data fabrication and/or falsification, double publication and/or submission, redundancy, etc.) have been completely observed by the authors.
Funding and support
This research resulted from an independent research without receiving any financial support.
Conflicts of Interest
Authors declared no conflict of interest.
Received: 2020/04/16 | Accepted: 2020/08/12 | Published: 2020/10/21
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |