BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
URL: http://journal.zums.ac.ir/article-1-6350-en.html


 , Mohammad Javad Behzadnia *2
, Mohammad Javad Behzadnia *2 

 , Zahra Bahari3
, Zahra Bahari3 

 , Mohammad Hossein Azimzadeh Ardabili1
, Mohammad Hossein Azimzadeh Ardabili1 


2- Trauma Research Center, Baqiyatallah University of Medical Sciences, Tehran, Iran ,
3- Dept. of Physiology and Medical Physics, Faculty of Medicine, Baqiyatallah University of Medical Sciences, Tehran, Iran
✅ Our data suggested that the older men and ischemic heart disease, hypertension and diabetes mellitus had a high risk of hospital readmission in COVID-19. The confirmed COVID-19 group showed a shorten time to be readmitted.
The coronavirus disease (COVID-19) is a highly pathogenic viral infection caused by severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2). Recently, it has caused major health concern due to the development of acute respiratory distress syndrome (ARDS) and high mortality rate in humans (1, 2). To date, there is no effective treatment against COVID-19 infection. Therefore, the prevention is considered as the most effective way to stop the fast spread of the infection (3). The management of COVID-19 is not well known. However, the assessment of clinical outcomes and related risk factors offer better prevention and management protocols for this novel infection. To our knowledge, the clinical outcome of COVID-19 infection in readmitted patients remains unknown in different areas of the world. Hospital readmission, as a costly public health concern, is related to a poor patient outcome (4). Additionally, hospital readmissions can put the patients at risk of hospital-acquired infections (5). It is well accepted that a period of self-isolation and post-discharge care management is effective for prevention of readmission. Readmission of patients with COVID-19 infection, may be due to several factors, including false negative RT-PCR, and unclear discharge criteria. Therefore, characterization of these patients with COVID-19 may inform post-hospitalization care (6, 7). Therefore, characterization of the risk factors of patients with COVID-19, who are re-admitted, is critical for clear discharge criteria and also post-discharge programming and care. The causes of hospital readmissions remain unclear. However, poor coordination and also poor follow-up care after discharge are considered as two main factors (5). Today, there is still no precise hospital guidelines on when an admitted patient with confirmed COVID-19 should be discharged. Therefore, physicians may discharge patients quickly, leading to worsening of the patient's outcome (8). Although the study of readmitted patients with COVID-19 is very important, to date very few studies have addressed COVID-19 readmissions (8). Jeon and colleagues in 2020 evaluated the relatedrisk factors leading to readmission in patients with COVID-19 in the Republic of Korea. They reported that the readmission rates of old age men, were higher. They also identified a higher risk of readmission in the patients with lopinavir/ritonavir therapy at the time of their first admission (9). Additionally, Li We and colleagues in 2020 explained that in a case of a “clinically cured” patient (a 41-year-old male) symptoms of COVID-19 reoccurred and real-time reverse transcription polymerase chain reaction (rRT-PCR) test was positive in the Fifth People’s Hospital of Chengdu City, China. They also reported that the length of stay and treatment course had been more than 35 days (10). Hence, it seems that understanding of the clinical characteristics of readmitted patients with COVID-19 can predict a hospital return of patients and optimize the health care. Several clinical studies and meta-analyses revealed the positive association between the routine laboratory data and the severity of COVID-19 infection. The most prevalent laboratory results in confirmed patients with COVID-19 are high level of erythrocyte sedimentation rate (ESR), C-reactive protein (CRP), and lactate dehydrogenase (LDH) (11). The present study was designed to assess the clinical data, biomarker levels and CT scan criteria in all readmitted patients in Baqiyatallah Hospital (Baqiyatallah University of Medical Sciences, Tehran, Iran) as a referral hospital between December 22, 2019 and June 20, 2020. For the better understanding of causes of readmission, we classified readmitted patients into three groups: (1) patients without COVID-19 infection, (2) patients with suspected COVID-19 infection, as well as (3) patients with confirmed COVID-19 infection. Additionally, we compared the clinical characteristics and risk factors for COVID-19 infection in all three groups. Indeed, the present study adds further evidence to characterization of the risk factors of patients with COVID-19 for preventing future hospital readmission.
Ethical considerations
The present retrospective study was approved by the Research Ethics Committee, Baqiyatallah University of Medical Sciences, Tehran, Iran (Ethical code: IR.BMSU.REC.1399.035).
Data collection
Data of all readmitted patients to Baqiyatallah Hospital (Baqiyatallah University of Medical Sciences, Tehran, Iran) from December 22, 2019 through June 20, 2020 were reviewed, retrospectively. Data were extracted for all readmitted patients including demographic data (age and gender), comorbidities, mortality rate, and length of hospital stay, as well as the length of days between two admissions (Table 1). Additionally, we extracted the variable results of laboratory data and respiratory imaging (CT results) of all readmitted patients at the first and second admissions (Tables 2 and 3). Based on their clinical data, all readmitted patients were divided to three groups as following: group 1 (without COVID-19 infection), readmitted patients without positive real-time reverse transcription polymerase chain reaction (rRT-PCR) test or without any other symptoms of COVID-19 infection such as fever, cough, dyspnea, chest pain, lack of appetite, lethargy, nausea, vomiting, diarrhea, headache, chills, sore throat, abdominal pain,and vertigo; group 2 (suspected COVID-19 group) readmitted patients with symptoms of COVID-19 infection (as their chief complain), but without confirmed test for COVID-19 infection such as RT-PCR test;group 3 (confirmed COVID-19 group) readmitted patients with symptoms of COVID-19 infection and positive RT-PCR or lung CT scan criteria for COVID-19 infection.
Statistical analysis
The present data were analyzed using the SPSS software (IBM. SPSS Statistic., version 24.0). Data were presented as mean ± standard error of the mean (SEM). The quantitative variables among the three groups were compared using one-way ANOVA analysis, followed by Tukey post-test. Qualitative variables were analyzed using Pearson's chi-squared test. For quantitative variables, data were presented by mean ± standard error of mean (SEM). For qualitative variables data were presented by frequency and percentage.
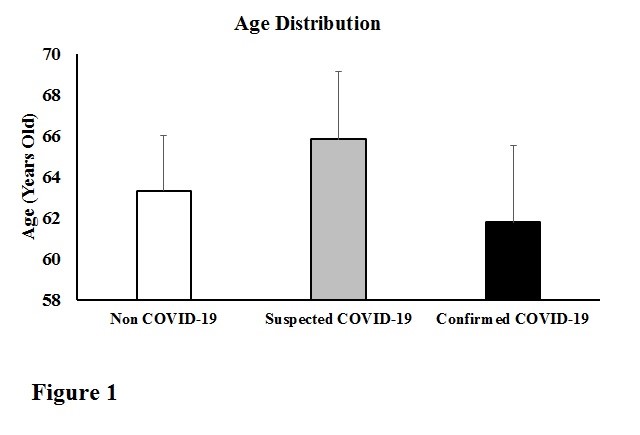
The mean ages of the readmitted patients were 63.31±2.69, 65.83±3.29, and 61.78±3.76 years in the three mentioned groups, respectively (Figure 1). Furthermore, the minimum age was 26 years and the maximum age was 98 years in non COVID-19 group. The minimum age was 21 years and the maximum age was 95 years in suspected COVID-19 group. The minimum age was 30 years and the maximum age was 93 years in confirmed COVID-19 group. There were no age differences between the three groups (P value=0.70).
Figure 1. Age distribution of all readmitted patients in three groups. Data were presented as mean±SEM. The one-way ANOVA analysis revealed no significantly differences between groups (P=0.70).
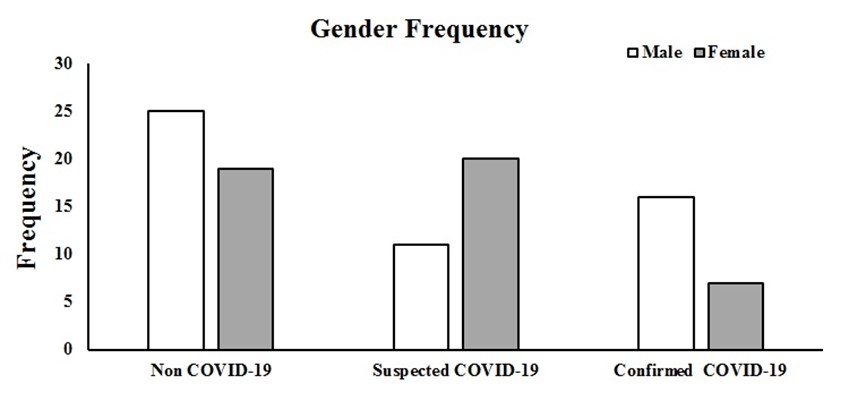
Additionally, gender of patients was significantly different between the three groups (Figure 2, P value =0.037). There was a lower percentage of female readmitted patients (30.4%) in the confirmed COVID-19 group as compared with the non COVID-19 group (43.2%) (Figure 2). Furthermore, our data analysis demonstrated that the length of hospital stay (days) in the first and second admissions were significantly different between the three groups (using one-way ANOVA analysis; P value =0.003, and P value =0.005, respectively). We observed significant differences between non COVID-19 group (0.91±0.09) and confirmed COVID-19 group (2.65±0.82) (P=0.002), and accordingly between the suspected COVID-19 (1.17±0.12) and confirmed COVID-19 groups (P=0.019) at the first admission.
Figure 2. Gender distribution of all readmitted patients in three groups. Data were presented as frequency. There was significantly differences between groups (P=0.037).
Additionally, we also showed a significant difference only between non COVID-19 group (1.00±0.09) and suspected COVID-19 group (2.29±0.35) (P=0.005) at the second admission. The Length between two admissions were significantly lower in the confirmed COVID-19 group (7.95±1.58) as compared to non COVID-19 group (13.71±1.49) and suspected COVID-19 group (13.03±1.47) (P=0.035, Table 1). Ischemic heart disease (22.72% vs. 9.67% vs. 34.78%; P=0.092) and hypertension (25.0% vs. 32.25% vs. 34.78%; P=0.627), as well as diabetes mellitus (13.63% vs. 38.70% vs. 26.08%; P=0.035) were more common among readmitted patients in the confirmed COVID-19 group (Table 1). However, other comorbidities such as gastritis, chronic lymphocytic leukemia (CLL), myelodysplastic syndromes (MDS), addiction, epidural hematoma (EDH), chronic kidney disease (CKD), Post-traumatic stress disorder (PTSD), subdural hematoma (SDH), respiratory, liver and renal diseases were not statistically significant (Table 1).
Table 1. Clinical characteristics of all readmitted patients. CLL: chronic lymphocytic leukemia, CKD: chronic kidney disease, EDH: epidural hematoma, ESRD: end-stage renal disease, MDS: myelodysplastic syndromes, PTSD: post-traumatic stress disorder, SDH: subdural hematoma.
Total of readmitted patients Non COVID-19 Suspected COVID-19 Confirmed COVID-19 P Value(N=98) (N=44) (N=31) (N=23) |
||||
Comorbidities-Frequency (%)Ischemic Heart DiesesHypertensionHypothyroidismDiabetes MellitusAnemiaGastritisCLLMDSEDHESRDLiver diseaseCancerAddictionPTSDBrain TraumaCKDRespiratory DiseaseParkinsonSDHRenal Disease |
10 (22.72%)11 (25.0%)1 (2.27%)6 (13.63%)8 (18.8%)1 (2.27%)1 (2.27%)3 (6.81%)1 (2.27%)3 (6.81%)2 (4.54%)11 (25.0%)2 (4.54%)1 (2.27%)1 (2.27%)0 (0.0%)0 (0.0%)1 (2.27%)0 (0.0%)0 (0.0%) |
3 (9.67%)10 (32.25%)3 (9.67%)12 (38.70%)2 (6.45%)1 (3.22%)0 (0.0%)0 (0.0%)0 (0.0%)0 (0.0%)2 (6.45%)3 (9.67%)0 (0.0%)0 (0.0%)0 (0.0%)4 (12.90%)2 (6.45%)3 (9.67%)1 (3.22%)0 (0.0%) |
8 (34.78%)8 (34.78%)1 (4.34%)6 (26.08%)2 (8.69%)0 (0.0%)0 (0.0%)0 (0.0%)0 (0.0%)1 (4.34%)1 (4.34%)2 (8.69%)0 (0.0%)0 (0.0%)0 (0.0%)0 (0.0%)2 (8.69%)0 (0.0%)0 (0.0%)1 (4.34%) |
0.0920.6270.330*0.0350.2780.6930.5440.1550.5440.3500.9030.1200.2920.5440.544**0.0090.1650.1360.3240.197 |
Length of hospital stayDay (Mean±SEM)First AdmissionSecond Admission |
(0.91±0.09)(1.00±0.09) |
(1.17±0.12)(2.29±0.35) |
(2.65±0.82)(1.93±0.52) |
**0.003**0.005 |
Length between two admission (day) |
(13.71±1.49) |
(13.03±1.47) |
(7.95±1.58) |
*0.035 |
OutcomeMortality |
1 (2.27%) |
3 (9.67%) |
6 (26.08%) |
*0.010 |
Patients who were readmitted in the non COVID-19 group had a lower mortality rate (2.27%) as compared with the suspected COVID-19 (9.67%) and confirmed COVID-19 (26.08%) groups (P=0.010, Table 1). In the first admission, laboratory abnormalities in the confirmed COVID-19 group included elevated CRP (20.33±5.57) and ESR levels (31.88±6.54). Similarly, in the second admission, laboratory abnormalities including elevated CRP (21.40±6.80) and ESR levels (40.17±7.50) were seen in the confirmed COVID-19 group. The WBC count in the confirmed COVID-19 group (5.93±0.59) was significantly lower than the non COVID-19 group (9.18±0.69) in the first admission (P=0.023, Table 2). Furthermore, in the first and second admissions, thet RBC coun and hemoglobin levels in the confirmed COVID-19 group were significantly higher than the non COVID-19 group (Table 2).
Table 2. Laboratory data and biomarker levels of all readmitted patients.
|
Total of readmitted patients Non COVID-19 Suspected COVID-19 Confirmed COVID-19 P Value (N=98) (N=44) (N=31) (N=23) |
||||
|
WBC Count WBC1 WBC2 |
(9.18±0.69) (8.95±0.62) |
(9.08±1.05) (8.94±0.76) |
(5.93±0.59) (7.97±1.03) |
*0.023 0.64 |
|
Lymphocytes Count Lymphocytes 1 Lymphocytes 2 |
(22.43±2.27) (24.05±3.00) |
(19.21±1.72) (24.39±3.68) |
(23.34±2.10) (20.87±2.92) |
0.31 0.76 |
|
Poly Poly 1 Poly 2 |
(69.90±2.62) (68.22±3.38) |
(71.70±2.63) (68.58±4.15) |
(70.60±2.61) (72.36±3.41) |
0.88 0.74 |
|
RBC Count RBC1 RBC2 |
(4.44±0.37) (3.98±0.17) |
(4.05±0.16) (3.96±0.14) |
(5.15±0.22) (4.83±0.24) |
*0.02 **0.003 |
|
HB Level HB 1 HB 2 |
(11.98±0.64) (11.14±0.53) |
(11.40±0.49) (11.02±0.38) |
(14.20±0.57) (13.49±0.62) |
**0.004 **0.003 |
|
ESR ESR 1 ESR 2 |
(49.62±9.38) (40.70±5.65) |
(39.34±6.47) (49.86±7.20) |
(31.88±6.54) (40.17±7.50) |
0.29 0.52 |
|
CRP Level CRP 1 CRP 2 |
(17.31±8.74) (30.48±11.42) |
(31.02±12.10) (48.31±12.06) |
(20.33±5.57) (21.40±6.80) |
0.53 0.15 |
The other biomarker levels were similar in the three groups. As shown in table 3, among all 98 readmitted patients, 25 patients had RT-PCR test in the first or second admission. Among 25 patients, 20 patients had positive RT-PCR results in the first admission and 17 patients had positive RT-PCR results in the second admission. Furthermore, among all 98 readmitted patients, 30 patients had a lung CT scan in the first admission and 31 patients had CT scan in the second admission. Generally, among 98 patients, only 23 patients (20 patients by positive RT-PCR test and 3 patients by positive CT criteria) had confirmed COVID-19 in the first and second admissions. Among all patients, 3 patients had positive CT scan criteria (indicated as confirmed COVID-19 cases). These 3 patients, did not have a RT-PCR test. Analysis of lung CT scan results in the first admission showed that a higher percentage of the patients had bilateral lung involvement (n=24) and also had GGO lesions (n=20) in the first admission. However, most of the patients had negative CT results for consolidation (n=22) and crazy paving (n=26) criteria in the first admission. Similarly, most of the patients who had taken CT scan in the second admission, had bilateral lung involvement (n=19) and also positive results for GGO criteria (n=20). However, most of the patients had also negative results for consolidation (n=24) and crazy paving (n=29) criteria in the second admission.
Table 3. The compound tomography criteria analysis for the confirmation of COVID-19 in readmitted patients.
|
Frequency Frequency |
||||
|
CT1 |
30 |
Involvement |
One side |
2 |
|
Two side |
24 |
|||
|
No involvement |
4 |
|||
|
GGO |
Positive |
20 |
||
|
Negative |
10 |
|||
|
Consolidation |
Positive |
8 |
||
|
Negative |
22 |
|||
|
Crazy Paving |
Positive |
4 |
||
|
Negative |
26 |
|||
|
CT2 |
31 |
Involvement |
One side |
5 |
|
Two side |
19 |
|||
|
No involvement |
7 |
|||
|
GGO |
Positive |
20 |
||
|
Negative |
11 |
|||
|
Consolidation |
Positive |
7 |
||
|
Negative |
24 |
|||
|
Crazy Paving |
Positive |
2 |
||
|
Negative |
29 |
|||
|
PCR1 |
25 |
Positive |
20 |
|
|
Negative |
5 |
|||
|
PCR2 |
25 |
Positive |
17 |
|
|
Negative |
8 |
|||
Discussion
In the present study (182 days), we investigated 98 readmitted patients ,44 cases with no COVID-19 infection, 31 cases with suspected COVID-19, as well as 23 cases with confirmed COVID-19 infection in a referral general Hospital, Tehran, Iran. Today, there are few studies regarding the risk factors among readmitted patients with confirmed or suspected COVID-19 infection. It is well accepted that hospital readmission is expensive and common. There is plenty of evidence suggesting that the age, gender, race, major surgery, comorbidities, length of hospital stay, lack of healthcare knowledge and quick discharge of patients are some important risk factors related to readmission (12). Additionally, in some studies, it has been reported that addiction and homelessness are related to a higher risk of readmission (13, 14). Although it is suggested that all of the mentioned factors have a critical role in readmissions of the patients, some medical physicians have still poor knowledge on predicting high risk factors for hospital readmission (12). In the present study, no age differences were observed between the three groups. However, there was a significant difference in gender between the groups. Indeed, men accounted for the highest percentage of readmitted patients with confirmed COVID-19 (69.6%). Contradictory to our study, Atalla and colleagues identified no age, gender or race differences in COVID-19 readmitted and non-readmitted patients (15). Similar to our study, Jeon et al., in 2020 reported that among 328 readmitted patients, the elderly men had a higher risk of hospital readmission (9). Additionally, Rokadiya and colleagues identified a marked gender distribution in 60% of the males (15/25) in the readmission group with confirmed COVID-19 vs. 58.8% male (429/729) in all confirmed COVID-19 cases (16). Noticeably, in the present study and based on differences in comorbidities, the ischemic heart disease (34.78%), hypertension (34.78%), and diabetes mellitus (26.08%) were more prevalent among the readmitted patients with confirmed COVID-19 infection. Similarly, hypertension (32.25%) and diabetes mellitus (38.70%) were more prevalent among the readmitted patients with suspected COVID-19 infection. Additionally, hypertension (25.0%), cancer (25.0%), ischemic heart disease (22.72%), anemia (18.8%), and diabetes mellitus (13.63%) were more prevalent among the readmitted patients without COVID-19 infection. Richardson and colleagues in 2020 revealed that the common comorbidities were hypertension (56.6%), obesity (41.7%) and diabetes mellitus (33.8%) among 5700 patients with COVID-19 in the New York City area (15). Posso and colleagues in 2020 reported that comorbidities such as heart failure and chronic kidney disease are related to an elevated risk of hospital mortality in patients with COVID-19 in Spain (17). Smith and colleagues in 2014 have suggested that attention to treatment of comorbidities in the post-discharge period is a critical factor for prevention of hospital readmissions (18). Higher length of hospital stay in the first admission was observed in the confirmed COVID-19 group. However, a higher length of hospital stay in the second admission was also observed in the suspected COVID-19 group. In the confirmed COVID-19 group, readmissions happened sooner after discharge (7.95±1.58). Indeed, in the confirmed COVID-19 group, the period between the two admissions was much shorter than the other two groups. It is suggested that quick discharge of patients was likely related to COVID-19 symptoms progression. Rokadiya and colleagues reported that the average time before being re-admitted to the hospital was 10 days in the patients with confirmed COVID-19 infection (16). Richardson and colleagues found that the mean time for readmission was 3 days in patients with confirmed COVID-19 infection (17). We found that the confirmed COVID-19 group had a higher mortality rate (26.08%). Accordingly, the lower mortality rate was seen in non COVID-19 group (2.27%). Furthermore, we observed that the inflammatory markers (CRP and ESR) significantly increased in all three groups in both first and second admissions. The WBC count was significantly lower in the confirmed COVID-19 group than in the other two groups in the first admission. Furthermore, the RBC count and hemoglobin level were significantly higher in the confirmed COVID-19 group than in the other groups in the first and second admissions. The other biomarkers were similar in the three groups. Similar to our study, Rokadiya and colleagues in 2020 reported that the biomarker levels were similar in readmitted COVID-19 group and COVID-19 discharged group (16). Additionally, our analysis of chest CT scan criteria and RT-PCR results in readmitted patients showed that, 20 patients had positive RT-PCR in the first admission and 17 patients had a positive RT-PCR in the second admission. Furthermore, among all 98 readmitted patients, 30 patients had CT scan in the first and 31 patients had CT scan in the second admission. Our CT scan results in the first admission represented that most of the patients had bilateral lung lesions (n=24) and also some evidence of GGO (n=20) in the first admission. However, a higher percent of patients had negative results for consolidation (n=22) and crazy paving (n=26) criteria in the first admission. Similarly, among 31 patients who had taken lung CT scan in the second admission, had a higher percent of bilateral lung lesions (n=19) and also positive evidence of GGO criteria (n=20) in the second admission. However, most of the patients had no evidence of consolidation (n=24) and crazy paving (n=29) in the second admission. Zhang and colleagues in 2020 evaluated CT scan results of 34 patients with confirmed COVID-19. They reported that 52.94% of the patients (n=18) had GGO lesions and only 3 patients had consolidation (19). They suggested that the bilateral positive lung GGO, air bronchogram, as well as enlarged vascularities are the early CT sacn criteria for COVID-19 infection. The present study suggested that ischemic heart disease, hypertension, and diabetes mellitus had a higher risk of hospital readmission in patients with COVID-19 infection. Targeting one hospital and small sample size are limitations of our study. Furthermore, the lack of follow-up of patients was another limitation of our study.
Conclusion
The present study suggested that the elderly men with ischemic heart disease, hypertension, and diabetes mellitus had a higher risk of hospital readmission. Additionally, hypertension, cancer, ischemic heart disease, anemia ,and diabetes mellitus were more prevalent among the readmitted patients without COVID-19 infection. The period between the two admissions was markedly shorter in the confirmed COVID-19 group than in the other two groups. It is suggested that quickly- discharged patients without further evaluations were likely to have symptoms progression. Furthermore, we observed that inflammatory marker levels (CRP and ESR) were markedly increased in all three groups in both first and second admissions. Most of the patients had bilateral lung lesions and also had positive results for GGO criteria of CT in the second admission. Finally, it is strongly recommended that the physician should focus more on high risk patients who have lung evidence of infection progression and avoid discharging the high risk patients with predisposed factors without further evaluation.
Acknowledgements
We would like to thank"Clinical Research Development Unit of Baqiyatallah Hospital" for financial support, guidance and advice.
Conflicts of Interest
The authors declare no conflicts of interest.
Received: 2021/01/2 | Accepted: 2021/06/10 | Published: 2022/04/1
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |