Sat, Jul 5, 2025
[Archive]
Volume 30, Issue 141 (July & August 2022)
J Adv Med Biomed Res 2022, 30(141): 385-387 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Samiee-Rad F. An Exceptional Occurrence of Uterus Mullerian Adenosarcoma in a Young Iranian Woman. J Adv Med Biomed Res 2022; 30 (141) :385-387
URL: http://journal.zums.ac.ir/article-1-6405-en.html
URL: http://journal.zums.ac.ir/article-1-6405-en.html
Dept. of Pathobiology, Clinical Research Development Unit, Kosar Hospital, Qazvin University of Medical Sciences, Qazvin, Iran , fsamieerad@gmail.com
Full-Text [PDF 507 kb]
(31541 Downloads)
| Abstract (HTML) (59900 Views)
Therefore, main diagnostic clue on low-power was the stromal cells periglandular cuffing (4-6). Above microscopic descriptions suggest that leaf-like pattern of stromal cells with mildly cellular pleomorphism and scant mitotic activity is in favor of low- grade adenosarcomas.
Atypical endometrial polyp showed incomplete or focally presence of histomorphologic criteria of mullerian adenosarcoma. So, accurate discrimination is a diagnostic challenge and definite diagnosis confirmed retrograde (3).
In initial presentation, our patient had a giant endometrial polyp. Therefore, one of the risk factors of uterus mullerian adenosarcoma may be a large endometrial polyp.
The level of accurate detection and management of low -grade adenosarcoma should be improved. Pathologists and surgeons at major gynecology referral treatment centers are much more likely to be familiar with low- grade adenosarcoma and its clinical awareness.
✅ Uterus mullerian adenosarcoma is a very rare malignancy. The clinical and Ultra Sonographic findings are not exclusive and the histomorphologic diagnosis of low-grade adenosarcomas is not straightforward. Herein, we present a young Iranian woman with menometrorrhagia due to exceptional occurrence of uterus Mullerian adenosarcoma.
Full-Text: (1036 Views)
Dear Editor
Uterus mullerian adenosarcoma is a very rare malignancy, commonly seen in perimenopausal and postmenopausal women (1). It is composed of biphasic growth patterns, including neoplastic mesenchymal and benign epithelial components (2).
The prevalence of mullerian adenosarcoma is rare and its occurrence in young female patients is a very exceptional event (1). The histomorphologic diagnosis of low-grade adenosarcomas is not straightforward and they are initially underdiagnosed as adenofibromas or endometrial polyps (3).
Therefore, in most cases, misdiagnosis can delay the appropriate therapeutic interventions. Consequently, it is important to detect low-grade adenosarcomas immediately after presentations.
A 24-year-old woman with menometrorrhagia for 8 months was referred without any personal risk factor and family history of malignancy. In the bimanual pelvic examination, the uterine indicated increased size. The ultrasound findings showed the enlargement of the uterus and a polypoid heterogeneous echo, M:53*40*20 mm2. She underwent hysteroscopy polypectomy. Histopathological findings showed endometrial polyp.
After 3 months, the patient was readmitted due to abnormal vaginal bleeding. The ultrasound disclosed enlargement of the uterus and a polypoid heterogeneous echo, M: 85*45*35 mm2. She underwent endometrial dilation and curettage. Histopathological findings showed hypercellular malignant infiltrative neoplasm in interlacing fascicular and storiform growth pattern. Individual mildly to moderately pleomorphic spindle- shaped tumor cells were characterized with a high N/C ratio, hyperchromatic nuclei, and eosinophilic cytoplasm with indistinct cell borders. Mitotic activities were about 30/10 HPF. The epithelial lining was benign-looking endometrial and endocervical epithelium. Tumor cells invaded into myometrium. Islands of cartilaginous tissue were seen (Figure 1A,B). Final diagnosis based on histology and immunohistochemical staining was adenosarcoma with sarcomatous overgrowth. Pelvic Magnetic Resonance Imaging (MRI) studies showed tumor involvement of upper part of cervix.
Therefore, in most cases, misdiagnosis can delay the appropriate therapeutic interventions. Consequently, it is important to detect low-grade adenosarcomas immediately after presentations.
A 24-year-old woman with menometrorrhagia for 8 months was referred without any personal risk factor and family history of malignancy. In the bimanual pelvic examination, the uterine indicated increased size. The ultrasound findings showed the enlargement of the uterus and a polypoid heterogeneous echo, M:53*40*20 mm2. She underwent hysteroscopy polypectomy. Histopathological findings showed endometrial polyp.
After 3 months, the patient was readmitted due to abnormal vaginal bleeding. The ultrasound disclosed enlargement of the uterus and a polypoid heterogeneous echo, M: 85*45*35 mm2. She underwent endometrial dilation and curettage. Histopathological findings showed hypercellular malignant infiltrative neoplasm in interlacing fascicular and storiform growth pattern. Individual mildly to moderately pleomorphic spindle- shaped tumor cells were characterized with a high N/C ratio, hyperchromatic nuclei, and eosinophilic cytoplasm with indistinct cell borders. Mitotic activities were about 30/10 HPF. The epithelial lining was benign-looking endometrial and endocervical epithelium. Tumor cells invaded into myometrium. Islands of cartilaginous tissue were seen (Figure 1A,B). Final diagnosis based on histology and immunohistochemical staining was adenosarcoma with sarcomatous overgrowth. Pelvic Magnetic Resonance Imaging (MRI) studies showed tumor involvement of upper part of cervix.
 |
 |
| A | B |
Figure 1. A and B. Histomorphologic results of adenosarcoma with sarcomatous overgrowth. The sarcomatous component and cartilaginous tissue. Hematoxylin and eosin staining, X10 (A) and X 400(B).
Chest and abdominal computed tomography (CT) scan showed no abnormality.
The patient underwent abdominal radical hysterectomy and pelvic lymphadenectomy. She was then referred to an oncologist and did not experience tumor recurrence in a 3-month follow-up.
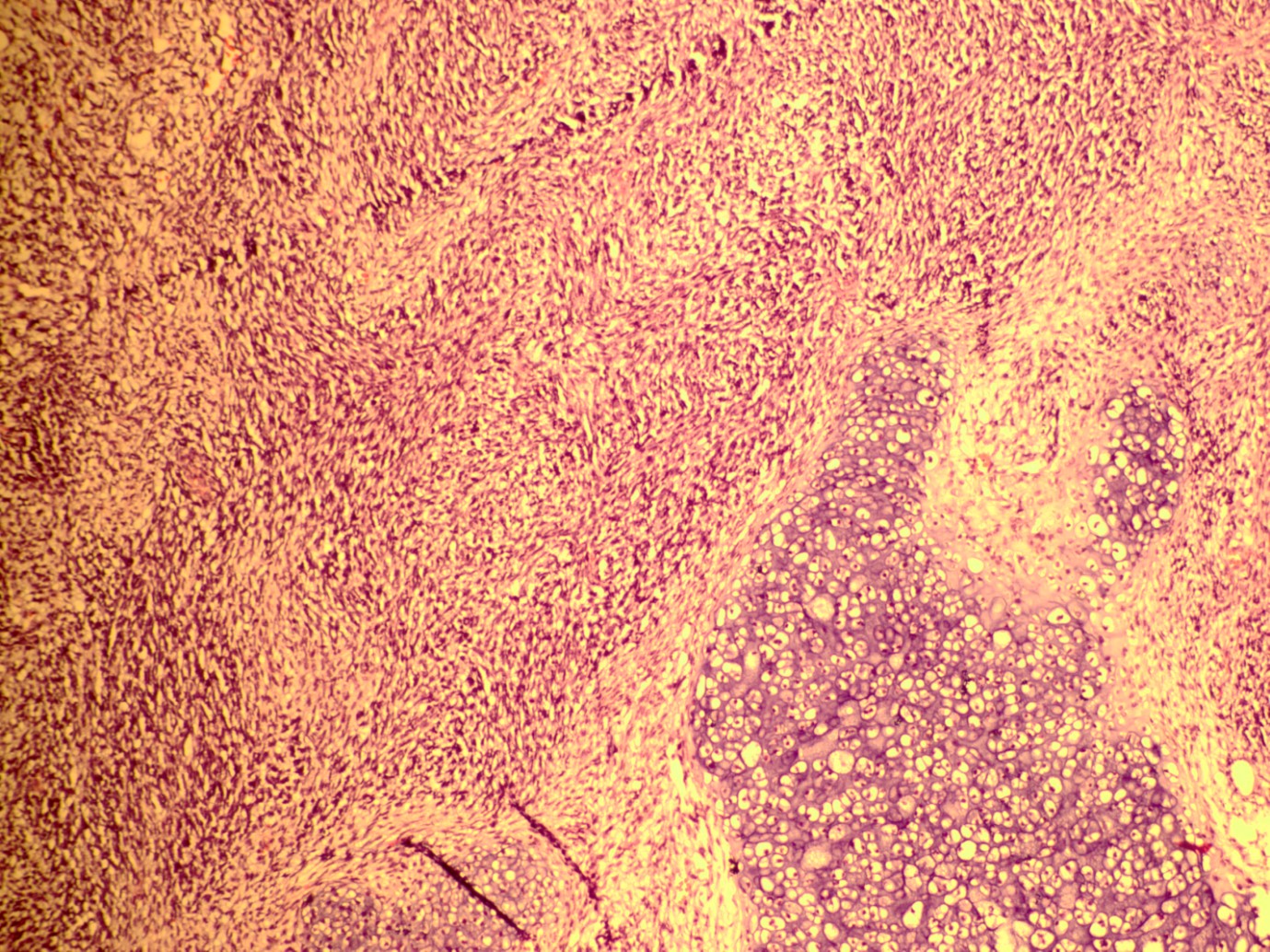
We reexamined the patient's previous pathology slides. There were a few large dilated cysts lined by benign endometrial epithelium, intraglandular papillaroid projections, surrounded by mildly increased cellular stroma demonstrating mild nuclear hyperchromasia and less than 2 mitotic figures per 10 HPF (Figure 2A,B).
The patient underwent abdominal radical hysterectomy and pelvic lymphadenectomy. She was then referred to an oncologist and did not experience tumor recurrence in a 3-month follow-up.
We reexamined the patient's previous pathology slides. There were a few large dilated cysts lined by benign endometrial epithelium, intraglandular papillaroid projections, surrounded by mildly increased cellular stroma demonstrating mild nuclear hyperchromasia and less than 2 mitotic figures per 10 HPF (Figure 2A,B).
 |
 |
| A | B |
Figure 2. A and B. Histomorphologic results of low grade adenosarcoma. The large dilated cysts lined by benign endometrial epithelium, and surrounded by mildly cellular stroma with mild atypia. Hematoxylin and eosin staining, X40 (A) and X 400(B).
Atypical endometrial polyp showed incomplete or focally presence of histomorphologic criteria of mullerian adenosarcoma. So, accurate discrimination is a diagnostic challenge and definite diagnosis confirmed retrograde (3).
In initial presentation, our patient had a giant endometrial polyp. Therefore, one of the risk factors of uterus mullerian adenosarcoma may be a large endometrial polyp.
The level of accurate detection and management of low -grade adenosarcoma should be improved. Pathologists and surgeons at major gynecology referral treatment centers are much more likely to be familiar with low- grade adenosarcoma and its clinical awareness.
Acknowledgements
None.
Conflicts of Interest
None.
Subject:
Clinical Medicine
Received: 2021/01/28 | Accepted: 2022/06/15 | Published: 2022/06/30
Received: 2021/01/28 | Accepted: 2022/06/15 | Published: 2022/06/30
References
1. Nathenson MJ, Ravi V, Fleming N, et al. Uterine adenosarcoma: a review. Curr Oncol Rep. 2016;18:68. [DOI:10.1007/s11912-016-0552-7] [PMID]
2. Liu H, Shen Z, Wu D, et al. Uterine adenosarcoma with sarcomatous overgrowth: a case report of aggressive disease in a 16-year-old girl and a literature review. Pediatr Adolesc Gynecol.2018;31:426-31. [DOI:10.1016/j.jpag.2017.12.012] [PMID]
3. Howitt BE, Quade BJ, Nucci MR. Uterine polyps with features overlapping with those of Müllerian adenosarcoma: a clinicopathologic analysis of 29 cases emphasizing their likely benign nature. Am J Surg Pathol. 2015;39(1):116-26. [DOI:10.1097/PAS.0000000000000303] [PMID]
4. Pinto A, Howitt B. Uterine adenosarcoma. Arch Pathol Lab Med. 2016;140(3):286-90. [DOI:10.5858/arpa.2014-0523-RS] [PMID]
5. McCluggage WG. A practical approach to the diagnosis of mixed epithelial and mesenchymal tumours of the uterus. Modern Pathol. 2016;29(1):S78-91. [DOI:10.1038/modpathol.2015.137] [PMID]
6. Tanveer N. Polypoid adenosarcoma of uterus with chondroid differentiation: A rare diagnosis. Indian J Pathol Microb. 2017;60(4):620. [DOI:10.4103/IJPM.IJPM_70_17] [PMID]
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |






