BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
URL: http://journal.zums.ac.ir/article-1-6591-en.html


 , Nasibeh Mohammadi *2
, Nasibeh Mohammadi *2 

 , Raheleh Kaviani1
, Raheleh Kaviani1 

 , Hamidreza Pouraliakbar3
, Hamidreza Pouraliakbar3 

 , Niloufar Parsa1
, Niloufar Parsa1 


2- Echocardiography Research Center, Rajaie Cardiovascular Medical and Research Center, Iran University of Medical Sciences, Tehran, Iran ,
3- Cardiovascular Imaging Research Center, Rajaie Cardiovascular Medical and Research Center, Iran University of Medical Sciences, Tehran, Iran
✅ We herein describe a 34-year-old woman with a persistent left superior vena cava (PLSVC) impinging on the posterior wall of the left atrium, subdivided by a membrane at the distal part of the impingement.
The Cor triatriatum is a rare congenital abnormality found incidentally in asymptomatic patients during echocardiography or evaluations for pulmonary arterial hypertension (1). The main feature of this abnormality is a fibrous membrane inside the left atrium (LA), dividing it into 2 posterosuperior and inferoanterior cavities. The upper cavity receives pulmonary venous drainage, and the lower one contains the LA appendage (2). These cavities are connected at the orifice, and the severity of the resulting stenosis and symptoms depends on the size of the orifice between the 2 LA parts (3). When the diameter exceeds 10 mm, patients are generally asymptomatic (4). The supramitral ring and the cor triatriatum may resemble each other in transthoracic echocardiography (TTE) and computed tomography. The difference, however, lies in the fact that in the cor triatriatum, the pulmonary veins are in the posterosuperior chamber and the LA appendage and the mitral valve are in the inferoanterior chamber, whereas in the supramitral ring, the LA appendage and the pulmonary veins are in the posterosuperior chamber and the mitral valve is in the inferoanterior chamber (1).
The supramitral ring is a subcategory of stenotic mitral valve lesions and may be associated with such other abnormalities as the ventricular septal defect, subaortic valve stenosis, parachute mitral valves, the cor triatriatum, and the persistent left superior vena cava (PLSVC) (5), with the latter being the most common congenital cardiac anomaly of them all.
The visualization of a dilated coronary sinus (CS) by TTE should place the PLSVC at the forefront of the likely diagnoses, although it is asymptomatic in most cases (2).
The concurrence of the aforementioned congenital diseases constitutes a rare condition, which makes our case scintillating. Furthermore, our case differs from the rare reported instances of the conventional association between these congenital anomalies insofar as in our patient, not only did a markedly dilated CS due to a PLSVC mimic the clinical and echocardiographic features of a cor triatriatum sinistrum (1, 2), but also the supramitral ring appeared as a nonobstructive ring attached to the atrial side of the mitral valve.
TTE, performed to evaluate possible structural heart diseases, revealed a left ventricular (LV) ejection fraction of 55% with a normal LV global function, a mild-to-moderate mitral insufficiency, and an enlarged LA (52 mL/m2) (Figure 1). Additionally, a thin, small indentation from the atrial side of the anterior mitral valve leaflet was visualized, suggesting a supramitral ring (Figure. 2).
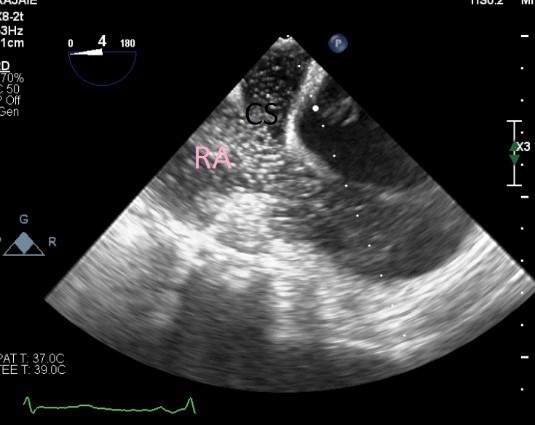
There was also a severely dilated CS, indicating the drainage of a PLSVC into the CS with turbulent flow across its length. The huge CS was responsible for the obstruction of the LV inflow tract, with a mean gradient of 3 mm Hg and the narrowest diameter of 9.3 mm. Injection of microbubbles intravenously in the left arm disclosed CS opacification, immediately followed by right-sided heart opacification, which confirmed the presence of the PLSVC and the dilated CS (Figure. 3).
Transesophageal echocardiography confirmed the findings of the TTE study. Computed tomography angiography showed a dilated LA, which contained a membrane-like structure, dividing it into proximal and distal chambers (Figure. 4).
 |
 |
| Figure 1. Transesophageal echocardiography shows an enlarged left atrium, a dilated coronary sinus (red arrow), a membrane-like structure (yellow arrow), and moderate stenosis along the dilated coronary sinus (blue arrow). (LA: left atrium, LV: left ventricle, RV: right ventricle) |
Figure 2. Transesophageal echocardiography illustrates a nonobstructive supramitral ring (white arrow). |
 |
 |
| Figure 3. The image shows the drainage of the dilated coronary sinus into the right atrium in contrast study. | Figure 4. Computed tomography angiography shows a dilated coronary sinus (blue arrow), resulting in a membrane-like structure in the left atrium. |
Discussion
This report describes our experience of an unusual case of a young woman whose echocardiographic examination in the parasternal long-axis and 4-chamber views showed LV inflow obstruction by a pseudo cor triatriatum sinistrum resulting from a PLSVC draining into a huge CS. Saline contrast echocardiography and cardiac computed tomography angiography confirmed the presence of the PLSVC draining into the giant CS.
The PLSVC is the commonest of the superior systemic vein malformations, occurring in about 0.4% of the general population and 4.3% of those affected by congenital heart diseases (6). The PLSVC drains mainly into the CS (62%) and less commonly into the LA (21%) or a common atrium (17%). In situs solitus, the PLSVC almost always drains into the CS. Drainage to a common atrium occurs with situs ambiguous and right isomerism. Most PLSVC cases with drainage into the CS are asymptomatic and usually found incidentally during surgery, invasive cardiovascular procedures, or cardiovascular imaging. Nevertheless, in the presence of an atrial septal defect, a partial LV inflow obstruction may lead to LA return diversion and, thus, left-to-right shunts and exacerbated clinical symptoms. Moreover, studies have reported a higher incidence of cardiac arrhythmias and conduction defects in patients with the PLSVC, which might be secondary to the stretching and fibrosis of the atrioventricular node or the His bundle by the dilated CS or the dysfunction of the associated sinus node (1, 2, 7).
Another diagnostic challenge is that a markedly dilated CS due to a PLSVC can sometimes mimic the clinical and echocardiographic features of a supramitral ring or a cor triatriatum, as was the case in our patient. A significantly dilated CS may even produce LV inflow obstruction and heart failure and, consequently, give rise to pulmonary hypertension; it should, therefore, be considered in the differential diagnosis of pulmonary hypertension in infants (2, 7).
Conclusion
We herein presented a case of a PLSVC draining into the CS, causing its severe dilation. The huge CS, in turn, led to the obstruction of the LV inflow tract, with a mean gradient of 3 mm Hg and the narrowest diameter of 9.3 mm. Furthermore, the patient also had a supramitral ring, which appeared as a nonobstructive ring attached to the atrial side of the mitral valve. These findings can explain the etiology of the patient’s symptoms and the echocardiographic appearance of a pseudo cor triatriatum sinistrum. The echocardiographic findings were subsequently confirmed by cardiac computed tomography angiography.
Since our patient was symptomatic, we planned to surgically direct the PLSVC into the right SVC, repair the excessively dilated CS and the enlarged LA, and excise the supramitral ring.
Acknowledgements
None.
Conflicts of Interest
There is no conflict of interest.
Received: 2021/07/19 | Accepted: 2022/06/20 | Published: 2022/10/10
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |