BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
URL: http://journal.zums.ac.ir/article-1-6636-en.html


 , Ramezan Ali Ataee2
, Ramezan Ali Ataee2 

 , Mahsa Ramezanpour3
, Mahsa Ramezanpour3 

 , Danial Chaleshi4
, Danial Chaleshi4 

 , Ehsan Rahmanian *5
, Ehsan Rahmanian *5 


2- Dept. of Medical Microbiology, Faculty of Medicine, Baqiyatallah University of Medical Sciences, Tehran, Iran
3- Dept.of Obstetrics and Gynecology, Shiraz University of Medical Sciences, Shiraz, Iran
4- Student Research Committee, Shahid Sadoughi University of Medical Sciences, Yazd, Iran
5- Dept.of Rheumatology, School of Hormozgan University of Medical Sciences, Bandar-e Abbas, Iran ,
✅ ESR and calprotectin did not show good power in predicting disease activity individually but they could have significantly high prediction potency combined.
Rheumatoid arthritis (RA) is an autoimmune disease defined by chronic synovitis and progressive joint destruction. This follows joint infiltration with inflammatory cells such as neutrophils and macrophages, which is coupled with the production of a large amounts of inflammatory mediators. The exact pathological etiology remains unclear, although cytokines and chemokines like tumor necrosis factor-alpha (TNF-α), interleukin-6, and macrophage inflammatory protein (MIP) play roles in the disease progression and severity. RA is more prevalent in the sixth decade of life, and women are affected two to three times more than men. Disability and loss of functional efficiency are among the consequences of the disease. Certain environmental triggers, genetic susceptibility (e.g., HLA-DRB 1), and history of autoimmune disease are some risk factors for RA (1,2).
RA presents as chronic symmetric polyarthritis with progressive involvement of the feet and hands. The common signs and symptoms are tenderness, stiffness, and swelling; although these are not specific for RA. Diagnosis is based on a combination of signs, symptoms, clinical examination, and laboratory data, comprising a wide spectrum of factors with a lack of specificity. Laboratory data include C-reactive protein (CRP), erythrocyte sedimentation rate (ESR), and some more specific tests like rheumatoid factor (RF), antinuclear antibodies (ANA), and anti-cyclic citrullinated peptide (anti-CCP). The detection of RA in its early stages is possible by employing clinical and serological measures. Early diagnosis coupled with a deep understanding regarding the pathological mechanisms and associated biomarkers can enable us to minimize adverse outcomes and ensure optimal treatment for individuals with RA (3,4).
S100A8/9 calcium-binding proteins known as calprotectin, monocyte membrane protein, and neutrophil cytoplasmic protein are released under stress or inflammatory conditions. They can be detected in serum or body fluids as useful inflammatory markers. Researchers have recently shown more interest in calprotectin because of its existence in a specific site of the synovial tissue, which is the same site of bone destruction and erosion in RA (5,6). As mentioned, RA is a chronic disease that needs to be followed up on throughout the patient’s life. Hence, in this study, we investigated calprotectin as a serological marker in the hope of establishing an adequate means of diagnosing RA and following up on patients.
This cross-sectional study included 32 RA patients who were referred to the rheumatology clinic of Baqiyatallah Hospital (Tehran, Iran) from 2019 to 2020. The study protocol was approved by the Ethics Committee of Baqiyatallah Hospital with (code: IR.BMSU.BAQ.REC.1399.059). RA patients between 18 to 60 years of age with more than a year after diagnosis and with fulfilment of the 2010 ACR/EULAR RA criteria were enrolled by convenience sampling. Concurrent involvement of other inflammatory diseases such as renal, hepatic, heart, or intestinal inflammatory disease were the causes for exclusion.
A rheumatologist after explaining the study and obtaining informed consent from all patients, performed clinical examinations and requested laboratory tests (anti-CCP, ESR, RF, CRP, and calprotectin). Laboratory tests were done in Baqiyatallah Hospital laboratory with gold standard kits. Every three months, serial visits were performed to follow up on the disease activity, treatment-progress, and side effects. The final visit was placed after a year with the same method as the initial visit.
Disease activity was assessed based on the Disease Activity Score 28 (DAS-28) for 28 joints, by using the number of tender and swollen joints, the CRP level, and a general health assessment on a visual analog scale. In this scale, also we can use the ESR instead of the CRP at the price of attaining less accuracy in estimating the disease activity. Typically, the scale is categorized into cured (DAS-28 ≤ 2.4), low (2.4 < DAS-28 ≤ 2.9), moderate (2.9 < DAS-28 ≤ 4.6), and severe (DAS-28 > 4.6) disease. When CRP is replaced by ESR, the classification changes as follows: cured (DAS-28 ≤ 2.6); low (2.6 < DAS-28 ≤ 3.2); moderate (3.2 <DAS-28 ≤ 5.1); and severe activity (5.1 < DAS-28) (7). Here, the ESR, CRP, RF, anti-CCP, and calprotectin levels were assessed. CALPROLAB kit (CALPRO AS company, Norway) were used to measure the CRP level via an enzyme-linked immunosorbent assay (ELISA) (7).
Data was written with the statistical program SPSS ver. 20 (IBM, USA) to perform analysis. Descriptive statistics were used to determine the mean, number, and standard deviation. For analytical statistics, distribution of difference between to sample of ESR, CRP, and DAS-28 was assessed by using the Wilcoxon signed-rank and Mann-Whitney test. ESR and calprotectin with DAS-28 correlation were assessed by using the spearman test. Also, logistic regression was used to estimating whether the calprotectin or ESR individually are relevant with DAS-28 or not and P-value below 0.05 was considered significant.
This study was conducted on 32 RA patients (24 women and 8 men), with mean age of whom was 57.12 ± 11.15 years. The clinical and laboratory information collected at the start and conclusion (after one year) of the study are summarized in Table 1. In terms of initial and final values, the mean CRP-based DAS-28 was 3.98 ± 0.77 and 3.27 ± 0.56, respectively, while the mean ESR-based DAS-28 was 4.04 ± 1.01 and 3.22 ± 0.85, respectively (Figure 1).
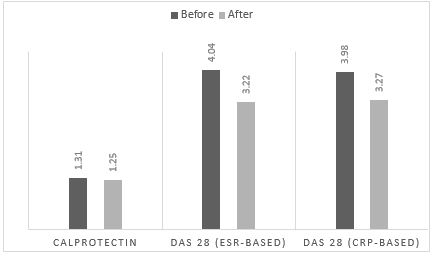
Figure 1. Comparisson Between CLP, DAS 28 before and after treatment
The changes over time were significant in both cases (P=0.00 and P=0.00, respectively), and a significant relationship was found between the quantitative scores of the two forms of DAS-28 (P<0.000); however, such significance was only seen after one year when comparing the categorized results of the CRP-based and ESR-based DAS-28 (P=0.00). Also, a significant change was seen in the CRP level over time (P=0.01) (Table 1).
Table 1. Clinical and laboratory data of patient
| P-value | After a year | Before | Laboratory dataa |
| 0.10 | 16.71 ± 15.76 | 22.06 ± 15.76 | ESR, mm/st hour |
| 0.01 | 10.91 ± 10.26 | 18.66 ± 15.31 | Mean CRP, mg/l |
| 0.91 0.06 0.08 0.00 0.00 |
88.00 ± 92.14 31 (96.8%) 1258.43 ± 76.87 3.27 ± 0.56 3.22 ± 0.85 |
138.34 ± 101.45 29 (90.6%) 1318.88 ± 132.51 3.98 ± 0.77 4.04 ± 1.01 |
Mean anti-CCPb, units/ml RF positivity, n (%) Calprotectin, ng/ml DAS-28 (CRP-based) DAS-28 (ESR-based) |
aData are mean ± SD or number (percent) and obtained at the beginning. b Anti-CCP: anti-cyclic citrullinated peptide.
The distribution of RA activity grade based on DAS-28 (CRP-based) was as follows: two patients (6.2%) with cured RA (3 patients when ESR based), one patient (3.1%) with low activity (same when ESR-based), 23 patients (71.8%) with moderate activity (24 patients when ESR-based), and 6 patients (18.7%) with severe activity (4 patients when ESR-based). As shown in Table 2, all patients had low or moderate disease activity based on the CRP-based DAS-28 after one year. However, at this time, the ESR-based DAS-28 indicated the presence of 8 patients (25%) with cured RA, 10 patients (31.3%) with low disease activity, 13 patients (40.6%) with moderate activity, and a patient (3.1%) with severe activity.
Table 2. Distribution of severity of RAa assessed by CRP-based DAS-28.
| After | Before | ||||
| Moderate | Low | ||||
| 2 (66.7%) | 1 (33.3%) | Low (3) | |||
| 13 (46.53%) | 10 (43.47%) | Moderate (23) | |||
| 2 (33.3%) 17 (53.1%) |
4 (66.7%) 15 (46.87%) |
Severe (6) Total b (32) |
|||
Data is given as count (percent) and is categorized based on DAS-28 classification; a RA, rheumatoid arthritis; b Changes in DAS-28 over time were significant (P=0.00).
Factors were assessed for correlations at separated times. At the both, the ESR correlated significantly with the CRP-based DAS-28 and the CRP level (at the beginning, P=0.00 and 0.01, respectively; after a year, P=0.01 and 0.00, respectively). Another significant correlation that was seen after one year was between the CRP level and the ESR-based DAS-28, yielding a P-value of 0.02. The correlation between the two forms of DAS-28 (ESR-based and CRP-based) was strongly significant (P<0.00). Notably, calprotectin did not show any significant correlation with either form of the DAS-28 quantitatively.
Ahead of logistic regression analysis on the after one-year CRP-based DAS-28 data, patients with cured disease or low disease activity were combined into one group. Accordingly, calprotectin was able to predict RA activity level to some extent (P=0.06), though a more efficient prediction was achieved when ESR and calprotectin were applied together (P=0.03) (Table 3).
Table 3. Status of laboratory parameters and their power to predict RA activity level.
| P-valueb | Prediction rate (%) | ||
| Moderate activity | Low activity | ||
| 0.07 | 52.9 | 60.0 | ESR |
| 0.06 0.03 |
76.4 82.4 |
46.6 80.0 |
Calprotectin ESR + Calprotectin |
Difference was calculated using Wilcoxon’s signed-rank test; blogistic regression was used to assess the prediction rate. ESR: erythrocyte sedimentation rate.
Discussion
The present study followed 32 RA patients over a one-year period and found a significant change in disease activity according to the CRP level as well as both forms of the DAS-28 (CRP-based and ESR-based). Although ESR did not change significantly over the time, it was correlated with the quantitative CRP-based DAS-28 and calprotectin level, but was not associated with the mean score of the two forms of the DAS-28 and the qualitative disease activity grades. Finally, only the CRP-based DAS-28 criteria were used to evaluate the predictive power of disease activity, as previous studies have shown that CRP is more efficient for this purpose. Also, ESR and calprotectin did not show good power in predicting disease activity individually but they could have significantly high prediction potency combined.
There are two types of accepted DAS-28 scoring systems: one makes use of the ESR while the other includes the CRP level. In the study of Roy M Fleischmann et al., the number of patients with high disease severity was higher, whereas this study revealed that after one year, only one patient had high disease severity according to the ESR-based DAS-28 while none had severe disease according to the CRP-based version. In the present study, a significant relationship was noted between the quantitative scores of the two forms of the DAS-28, with similar results having been reported in other studies. However, unlike those studies, when the disease severity was categorized based on the DAS-28 cut-off points, a significant relationship was only found between the qualitative results of the two forms of the DAS-28 when analysing the after one-year data, and not when analysing the initial data (7–10). These differences could be due to the higher rate of patients classified as having severe disease in DAS-28 (before) relative to the two forms of DAS-28. Nonetheless, in the study of Ashutosh Tamhane et al., the different forms of the DAS-28 had significant relationships with one another both quantitative and qualitatively (11).
In the present study, in agreement with the research of Roy M Fleischmann et al. and Ashutosh Tamhane et al., the mean ESR-based DAS-28 was higher than that of the CRP-based DAS-28, with previous studies suggesting that the latter underestimates disease severity (9,11).
This investigation was conducted with the aim of determining the relationship between serum calprotectin level and RA disease activity. To date, several studies have indicated a fairly remarkable relationship between the mentioned variables (12–15). Previous studies have also suggested the use of calprotectin for following up on RA patients and assessing their response to treatment, indicating an association between lower calprotectin levels and decreased disease severity based on DAS-28 (15–18).
Notably, calprotectin also did not show a significant relationship with any of the other laboratory parameters, which contradicts the results of some previous studies. In fact, in the study of Agrawal S et al., a significant relationship was observed between calprotectin and RF, while in the Hammer HB et al. study, calprotectin was significantly correlated with anti-CCP (19,20).
Ultimately, in addition to some clinical research, biological studies also confirm the hypothesis of a link between calprotectin and RA disease activity given the inflammatory nature of the disease. As a matter of fact, aggregated data confirms the power of this factor in predicting RA disease activity (21–24).
The key limitation of this study was the low number of subjects. This was because of COVID-19 pandemic situation caused lowering of referred to health care centers. One way that this issue undeniably affected the study outcomes was that the number of patients classified as having low or high disease severity was low.
Conclusion
The current study revealed no significant relationship between serum calprotectin level and the scores of either form of DAS-28 but when ESR and calprotectin were applied together was able to predict RA activity level.
Acknowledgements
The authors were greatly thankful for the spiritual support of the rheumatology clinic of Baqiyatallah Hospital, Tehran, Iran and its personnel collaborations.
Conflicts of Interest
The authors declare no conflict of interest.
Received: 2021/07/23 | Accepted: 2022/01/18 | Published: 2022/04/1
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |



