BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
URL: http://journal.zums.ac.ir/article-1-7626-en.html
2- Department of Dermatology , Vali-e-Asr hospital, School of Medicine, Zanjan University of Medical Sciences, Zanjan, Iran
3- Department of Clinical and Anatomical Pathologist, Bahar Medical Laboratory, Zanjan, Iran
Medicinal leech therapy (MLT) or Hirudotherapy (leeching using Hirudo medicinalis) is an ancient therapeutic modality that has regained popularity for managing conditions such as chronic pain, venous congestion, and osteoarthritis (1, 2). Medicinal leech therapy has received FDA approval in reconstructive plastic surgery since 2004 (1). Although generally safe, it has been associated with complications, including bacterial infections (most notably by Aeromonas species), localized hypersensitivity reactions, bleeding, and rarely pseudolymphoma (1).
Cutaneous pseudolymphoma (CPL) encompasses a group of benign reactive lymphoproliferative disorders that mimic cutaneous lymphoma clinically and histologically. Various triggers, including infections, trauma, tattoos, insect bites, acupuncture, and certain medications, have been implicated in its pathogenesis (3). CPL is often presented as pruritic firm red or brown-purple nodules or papules. The condition is diagnosed through clinical and histopathological correlation. CPL is reported in a few cases as a complication of MLT that appeared at the site of a leech application.
We found only 10 similar case reports in medical databases (4-13). This finding shows the rarity or underreporting of CPL induced by leech therapy. Here, we reported a case of CPL in a 55-year-old woman following leech therapy for knee pain and swelling.
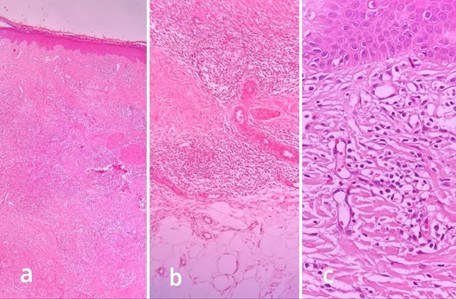
Figure 2. a) Acanthotic hyperkeratotic epidermis, dense perivascular and interstitial infiltration of lymphohistiocyts and eosinophils throughout dermis (H&E ×40). b) Extension of infiltrate to superficial subcutis (H&E ×100). c) Interstitial and perivascular infiltrate of lymphocytes, histiocytes, and eosinophils in the dermis (H&E ×400).
The patient was initially treated with topical fluocinolone acetonide and oral cetirizine.This regimen provided partial improvement. However, despite continued treatment, the lesions recurred at the same sites after three weeks. Subsequently, intralesional triamcinolone acetonide injection and cryotherapy targeting the persistent nodules were administered. Two weeks after this treatment, all lesions resolved. No recurrence was observed during the follow-up visits.
Discussion
CPL is a benign reactive lymphoproliferative disorder that closely resembles cutaneous lymphoma clinically and histologically. Firm red or brown-purple nodules or papules characterize it. Pruritus is a common symptom, although cases vary in their presentations, including asymptomatic or painful nodules. Histopathological analysis of these lesions typically reveals dense perivascular, superficial, and deep dermal lymphocytic infiltrates mixed with other inflammatory cells such as eosinophils, histiocytes, and plasma cells. Epidermal changes like hyperkeratosis and focal spongiosis are variably present (3).
Various triggers, including infections, trauma, tattoos, insect bites, acupuncture, and certain medications, have been implicated in its pathogenesis (3).
CPL is also a rare complication of leech therapy that was first reported by Smolle et al. in 2000 at the site of a leech application (4). Leech saliva contains several bioactive compounds, such as hirudin (an anticoagulant), calin (an anti-platelet), and hyaluronidase, which contribute to its therapeutic effects (2). The development of CPL following MLT may occur due to immune activation by the bioactive substances in the leech saliva or the physical trauma associated with leech application (2, 3).
In the process of a focused literature review in the reliable and accessible medical databases, we found only 10 similar case reports (4-13).
Reported cases in the literature suggest that leech-induced CPL can occur several weeks to several months after MLT. Most of the cases were women (8 out of 10 patients). The age range of patients was 22 to 77 years old (4-13). It has been associated with various uses of leech therapy, including for venous insufficiency (4, 11), fibromyalgia (7), pain management (6, 9), acne vulgaris (13), uterine myoma (8), and cosmetic purposes (5).
While most of the reported cases improved with corticosteroids (topical and intralesional), some studies have incorporated cryotherapy as part of the therapeutic approach, such as Tupikowask et al (8), Aktas et al (9) and Sadati et al (11).
Our case was a 55-year-old woman whose lesions appeared two weeks following MLT but responded partially to topical fluocinolone acetonide and oral cetirizine. Recurrence of lesions after three weeks indicated that a more aggressive treatment approach is necessary. Intralesional steroids such as triamcinolone acetonide are commonly used in the management of CPL, especially when lesions are persistent or recurrent. Cryotherapy is another option for localized lesions, providing an additional modality for reducing the size of nodules and promoting regression (14). In our patient, the combination of intralesional triamcinolone acetonide and cryotherapy led to the complete resolution of lesions; no recurrence was seen in the follow-up visits.
Conclusion
In conclusion, while CPL is a rare complication of leech therapy due to the increasing use of MLT in conventional medicine, especially for reconstructive surgery and pain management, clinicians must be aware of this potential adverse effect.
Declarations
Acknowledgements
We would like to thank the paitient for participating in this case report.
Ethical Considerations
Not applicable.
Authors' Contributions
Ali Sayyadinejad: Contributed to the study design, data collection, analysis and writing of the manuscript. Sahar Hoseinkhani: Assisted in data analysis and manuscript drafting. Abdolhakim Aghatabay: Performed the histopathological analysis. The final manuscript was read and approved by all of the authors.
Conflicts of Interest
The authors declare that there are no conflicts of interest.
Fund or Financial Support
This research received no specific grant from any funding agency in the public, commercial, or not for profit sector.
Using Artificial Intelligence Tools (AI Tools)
The authors were not utilized AI Tools.
Received: 2024/12/12 | Accepted: 2025/02/23 | Published: 2025/03/13
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |