BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
URL: http://journal.zums.ac.ir/article-1-6372-en.html


 , Mahdiyeh Meydanloo2
, Mahdiyeh Meydanloo2 

 , Sattar Jafari2
, Sattar Jafari2 

 , Saeed Mansouri Hashchin2
, Saeed Mansouri Hashchin2 

 , Mohammad Jafari3
, Mohammad Jafari3 

 , Negin Parsamanesh *4
, Negin Parsamanesh *4 


2- Dept. of Internal Medicine, School of Medicine, Zanjan University of Medical Sciences, Zanjan, Iran
3- Isfahan Gastroenterology and Hepatology Research Center, Isfahan University of Medical Sciences, Isfahan, Iran
4- Zanjan Metabolic Diseases Research Center, Zanjan University of Medical Sciences, Zanjan, Iran ,
✅ The 2019 Coronavirus disease pandemic (COVID-19) has spread to over two hundred countries worldwide, affecting > 170 million people and causing >3,500,000 deaths (May 29, 2021). Severe COVID-19 disease mostly disturbs the respiratory system, but gastrointestinal symptoms, including vomiting, nausea and diarrhea, are also present. Herein, we are reporting a COVID-19 patient with acute pancreatitis (AP) in Zanjan, Iran.
The global pandemic of Coronavirus disease-2019 (COVID-19) has reached over two hundred countries worldwide, affecting > 170 million people and causing > 3,500,000 deaths (May 29,2021) (1, 2). The severity of the illness varies from subclinical infections to the serious disease that requires hospitalization (3, 4). Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) mostly impacts the respiratory system, but there are also gastrointestinal signs, such as vomiting, nausea, and diarrhea (5, 6). Abdominal pain is prevalent in chronically- ill cases (7, 8). Viral RNA has been detected in fecal specimens and in gastrointestinal epithelial cells, indicating a potential path of fecal-oral transmission (9, 10). The most frequent gastrointestinal source of hospitalization in the United States is severe pancreatitis (11, 12). Acute pancreatitis formation is multifactorial, involving susceptibility and related damage (13). Gallstones and alcohol consumption are the most
prevalent causes, however; virus-induced acute pancreatitis has also been identified.
Documents were collected from a patient admitted to the Intensive Care Unit with COVID-19 at Valiasr hospital in Zanjan province of Iran in October 2020. Acute pancreatitis was diagnosed based on the Atlanta category. Swab samples and tracheal aspirates were taken from the patient. Blood testing including C- reactive protein (CRP), creatine kinase plus myoglobin, aspartate aminotransferase (AST) alanine aminotransferase (ALT), lactate dehydrogenase (LDH), D-dimer, and creatine phosphokinase levels and also diagnostic imaging were carried out.
A 28- year-old obese (BMI = 42) male presented with acute abdominal pain, vomiting, weakness, nausea, decreased appetite and abdominal function for days. The case complained of severe generalized abdominal pain especially in the Right Upper Quadrant (RUQ) and epigastric region radiating to the back for 4 days. He was not taking any medicine and did not have a history of alcoholism and smoking. Physical examination upon arrival indicated blood pressure of 110/70 and temperature of 37° C.
Abdominal laboratory workup is summarized in table 1. The patient’s amylase was increased beyond the normal level(ULN=90). AST and ALT, triglyceride, and lipase levels were normal. Chest CT scan indicated perioral ground- glass opacity in RML, RUL LUL (Fig a and b). Plural effusion collapse, consolidation, and atelectasis in the posterior of RLL on abdominal CT scan and severe inflammation were seen in the fat around the pancreas and the fat stranding in the kidneys especially on the left. The size of para -aortic infiltrates was normal and the pancreases showed heterogeneousdensity. The above symptoms can indicate necrotic pancreatitis.
Table 1. Laboratory testing results at the time of admission
| Laboratory experiment | Result |
| White cell count (per mm3) | 19/3 |
| Differential Count total neutrophils (per mm3) | 87/3 |
| Total lymphocytes | 10/3 |
| Platelet Count (per mm3) | 5000 |
| Hemoglobin (g/liter) | 18/3 |
| INR | 1.0 |
| Creatinine (μmol/liter) | 1/3 |
| Albumin (g/liter) | 3/4 |
| Blood urea Nitrogen | 27 |
| Triglyceride (mg/dl) | 143 |
| LDH | 2044 |
| Amylase (U/liter) | 83 |
| Magnesium (U/liter) | 2/2 |
| Total Bilirubin (mg/dl) | 0/9 |
| Direct Bilirubin (mg/dl) | 0/2 |
| C-reactive protein (mg/liter) | 5 |
| Alanine aminotransferase (U/liter) | 37 |
| Aspartate aminotransferase (U/liter) | 36 |
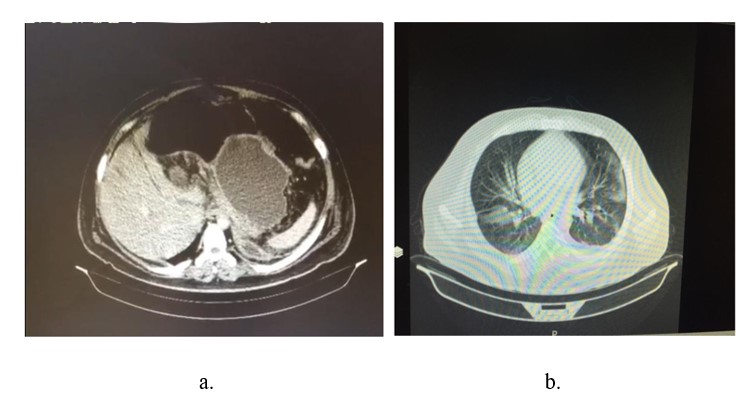
Figure 1. a. Inflammation in pancrease parenchyma on CT scan, b. Pulmonary consolidation compatible with Covid-19
The patient was identified with severe acute necrotizing pancreatitis with acute respiratory distress syndrome (ARDS).This happens when fluid builds up in the tiny, elastic air sacs (alveoli) in patients lungs. Then, the patient was admitted to the intensive care unit. He was cured symptomatically with bowel rest, intravenous crystalloid fluid resuscitation, and empirical antibiotics.The patient was RT-PCR positive for COVID- 19. The patient developed acute hypoxic respiratory failure needing high flow oxygen supplementation.
Discussion
Coronaviruses are a wide group of single-stranded RNA viruses. In humans, the virus frequently produces respiratory symptoms as well as myalgia. Our patient was PCR positive and had no other indications for pancreatitis such as gall stones, alcohol use, or medication intake .According to the COVID-19 and gastritis final symptoms evidence the patient most likelyhad pancreatitis in the context of corona virus. A number of etiological causes leading to acute pancreatitis have been identified. Gallstones and excessive alcohol intake are the most prevalent causes of acute pancreatitis. In 10%–20% of patients, an etiological component cannot be found. Several infectious agents, such as parasites, bacteria and viruses are recognized to infect the pancreas. Numerous gastrointestinal symptoms have been observed in COVID-19 patients. Mach et al., reported a 37- year- old woman with concomitant respiratory and gastrointestinal symptoms pancreatitis in the context of COVID 19. Also, absence of additional etiologies would recommend coronavirus–induced acute pancreatitis. In another study, it was reported that COVID-19 patients showed the pancreatic injury known by any abnormalities in amylase / lipase in less than 20% of cases (1). Some evidence has confirmed that COVID-19 could be related with gastrointestinal symptoms including abdominal pain (2-4) with identification of viral RNA in gastrointestinal tract (5-9).
Many variables such as pancreatic autodigestion, system complement, and enzyme activation, could induce acute pancreatitis activation. The hypothesis of microcirculation disruption, showed elevated leukocytes and pancreatic acinar cell necrosis and apoptosis (14). Viral pancreatitis occurs potentially due to the overt degradation via inflammatory and edema of pancreatic acinar cells. Additionally, damage by the virus to the pancreatic acinar cells may result in elevated intracellular enzyme or induce an apoptosis phase (14). COVID-19 pathogenesis is suspected to be regulated by the target cells' angiotensin-converting enzyme-2 (ACE-2) receptor, which is strongly expressed in the pancreatic cells (15). Thus, the cases presented highlight the significance of amylase or lipase measurement in patients with SARS-CoV-2 infection, particularly if patients suffer stomach pain.
Conclusion
None.
Acknowledgements
None.
Conflicts of Interest
None.
Received: 2021/01/14 | Accepted: 2021/06/24 | Published: 2022/04/1
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |



