BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
URL: http://journal.zums.ac.ir/article-1-6430-en.html
2- Clinical Research Development Unit, Imam Hossein Hospital, Shahroud University of Medical Sciences, Shahroud, Iran
3- School of Medicine, Shahroud University of Medical Sciences, Shahroud, Iran
4- Dept. of Epidemiology, School of Public Health, Shahroud University of Medical Sciences, Shahroud, Iran ,
✅ This case study includes three pregnant women with COVID-19 diagnosed during pregnancy or delivery between March 28 and May 13, 2020. All cases were confirmed by a positive pharyngeal reverse transcription polymerase chain reaction (RT-PCR) test and one case by computed tomography scan (CT Scan) in addition to the (RT-PCR).
The emergence of the novel coronavirus infection began in Wuhan, China, in December 2019 and spread rapidly as a threat to all regions of the world (1). In March 2020, the World Health Organization declared the disease a pandemic (2). Covid-19 disease can be fatal in severe cases. Initially, studies on the genetic, virology, epidemiology, laboratory, radiological and clinical characteristics of the disease in the population were conducted (3) , but then the effect of this disease on pregnant women and transmission through the placenta and various hypotheses were considered by researchers, taking into consideration that Covid- 19 infection in pregnant women can cause severe pneumonia, death and pregnancy complications including chorioamnionitis, eclampsia, premature birth, intrauterine growth restriction and other adverse pregnancy outcomes (4).Physiological, anatomical and immunological changes in pregnancy have systemic effects on the respiratory and cardiovascular function of pregnant women (5). These changes include variations in heart rate, decreased lung capacity and weakened immune system (6). Other anatomical changes such a increased transverse diameter of the thoracic cage and an elevated level of the diaphragm, decrease maternal tolerance to hypoxia. These changes when exposed to respiratory infections cause respiratory system dysfunction of the pregnant women and increase their morbidity and mortality (5).
Studies conducted in the world have shown that respiratory infections, including SARS, MERS, and influenza, increase the risk of death in pregnant women. These diseases also cause miscarriage, growth retardation and preterm birth (3), but no vertical transmission of SARS, MERS and influenza from the infected mother to the fetus has been observed (7, 8). Studies have also shown that changes in a woman's cardiovascular system and immune system increase her susceptibility to severe COVID-19 and due to the weakened immune system, these women may have no clinical symptoms and their diagnosis and treatment may be delayed (9, 10).
Study design and participants
The first case
The first patient was a 27-year-old woman gravid 2, Para 1 at 39 weeks and 5 days gestation and was admitted to Bahar Hospital on May12 to terminate her pregnancy on 13 May.
No history of contact with an infected person was reported. Without a history of underlying disease, vital signs including pulse rate, respiratory rate, and blood pressure were normal on admission. (Table.1).
Table1. Basic characteristics and laboratory results of pregnant women with coronavirus
| Maternal characteristics AND outcome | Case1 | Case2 | Case3 |
| Signs and symptoms on admission | Decreased sense of smell and taste | Cough fever |
No symptom |
| Gestational age (Week) | 39+5th week | 38 weeks | 39th weeks |
| Gravid, Para | 2,1 | 3,0,2 | 1,0 |
| History of abortion | NO | YES | NO |
| Comorbidities | NO | NO | NO |
| Type of delivery | Vaginal | Caesarean | Caesarean |
| Neonatal pneumonia | Negative | Negative | Negative |
| Type of diagnosis | Positive RT-PCR | Chest CT typical features | Positive RT-PCR |
| Vital signs | T=36.5 oC PR:80 BP:100/70 mm Hg) RR:17 |
T=38 oC PR:90 BP:110/70 mm Hg). RR:20 |
T=36.9 oC PR:88 BP:110/70 mm Hg) RR:19 |
| O2 Sat, % (SaO2) | 96% | 93% | 97% |
| Neonatal outcomes | Alive | Alive | Dead |
According to the electronic file during pregnancy care in the health center, she had not lost any unwanted weight during the last three months. No anorexia or reduced food intake was reported.
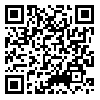
The results of laboratory tests and sonography were completely normal. Anomaly scan revealed normal anatomy and fetal growth in the second trimester of pregnancy. (Table 2) The growth chart of the pregnant mother is shown in Figure 1. The temperature was normal at the early hours of admission (T: 36.5 oC), but after 3 hours it reached 38 oC. According to the physician's instructions Apotel (acetaminophen) with serum sodium chloride was injected and the patient's temperature returned to 36.9 oC.
The nurse’s initial assessment form, including evaluation of health and disease history,and drug allergies was completed and the patient was normal in terms of level of consciousness, drug sensitivity and the nervous, urogenital, cardiovascular, respiratory and psychological systems, although the patient complained of decreased sense of smell and taste five days before her hospitalization.
The SARS-CoV-2 PCR test was ordered by the physician and the result was positive.
The patient was transferred to the isolation ward. After consultation and confirmation of two infectious disease specialists, Hydroxychloroquine Sulfate 200 mg (twicedaily for 5 days), was prescribed for the patient.
Vaginal delivery was performed on the afternoon of May13. After delivery, the patient was transferred to the maternity isolation ward again. The patient’s general condition, vital signs, and oxygen saturation (spo2=98%) indicated normal status. Medications prescribed during the period of hospitalization were antibiotics and anti-inflammatory drugs including Cefazolin 1 gr, diclofenac sodium 50 mg, Misoprostol 200, oxytocine 10u/ml.
Complications of labor including premature rupture of membranes, abnormal bleeding,and chorioamniotitis were not observed.
A boy neonate weighing 3,500g was born by vaginal delivery without any fetal distress. Apgar scores at one and five minutes after delivery were 9 and 10, respectively.
To prevent possible risks of transmission from mother to infant, no skin-to-skin contact between mother and baby was established.
The infant was separated immediately to avoid transmission and transferred to the neonatal ward (NICU) for initial care, and was not breastfed because of the potential risk of infection. All the necessary tests and examinations were performed for the infant; and the placenta was sent to a laboratory for pathology.
Table2. Laboratory and serological characteristics of pregnant women with coronavirus
| Laboratory characteristics | Case1 | Case2 | Case3 |
| WBC(mm^3, normal range 4000-10000) | 6200 | 6700 | 9200 |
| RBC (10^6/ul, normal range 4-6) | 3.63 | 4.35 | 3.44 |
| Hb(g/dl, normal range 12.5-14) | 10.2 | 14.4 | 11.5 |
| Hct(%) | 45.4 | 40.1 | 31.4 |
| MCV(Fl, normal range 80-100) | 105 | 92 | 91 |
| MCH(Pg, normal range 27-32) | 28 | 33 | |
| MCHC(%gr, normal range 31-35) | 33 | 36 | 36 |
| Platelet(mm^3, normal range 150000-450000) | 208000 | 222000 | 150000 |
| CRP( Mg/L, normal range negative) | Positive 1+ | Slightly positive | Slightly positive |
| Creatinine(Mg/dL, normal range 0.6-1.1) | 0.9 | 1 | 0.9 |
| AST (U/L, normal range <31) | 19 | 25 | 30 |
| ALT (U/L, normal range <31) | 14 | 15 | 13 |
| LDH(U/L, normal range 64-306) | 373 | 320 | 406 |
The second case
The second patient, a 34-year-old woman (Gravid 3, Para 0, Ab2), was admitted with a gestational age of 38 weeks on 28 March. Vital signsincluding pulse rate, respiration and blood pressure were normal on admission. (Table 1)
Pregnancy care at the health center did not report any unwanted weight loss or anorexia over the past three months. The growth chart of the pregnant mother is shown in Figure 2.The results of blood tests and ultrasound were completely normal. Morphology scan revealed normal anatomy and fetal growth.
The patient complained of a 24-hour fever, dry cough but there was no history of exposure to a person infected with SARS-CoV-2. The temperature on admission was 38 oC.
The PCR test result was positive, so COVID-19 was confirmed. In addition, after delivery a chest radiography was performed on March 29, which showed multiple diffuse patchy glass opacities in both lungs. Treatment with Hydroxychloroquine 200 mg was started for two weeks
Cesarean section was performed because of abnormal labor (insufficient strength of uterine forces and no dilatation of cervix) and after delivery, the patient was transferred to an isolated ward and treated with medications. No delivery complications were observed. Blood pressure was checked every half hour. Medication instructions during hospitalization included cefazoline, clindamycin, gentamycin, apotel, and diclophenac.
A 3,600g boy neonate was born by cesarean section on March29, at 38 weeks gestation with a normal and transparent amniotic volume. Apgar score at 1 and 5 minutes were 9 and 10, respectively. No asphyxia was observed in the neonate. There was no skin-to-skin contact between the mother and baby. Breastfed wasnot used because of the potential risk of infection. The neonate was transferred to the neonatal ward (NICU) for initial care. The neonate sample was negative for SARS-CoV-2.
The third case
The third patient was a 25-year-old woman (gravid 1, Para 0) with a gestational age of 39+2 weeks, who was admitted on May 10.She reported a history of exposure to the contaminated environment and the infected person on April 24, but she was in good general condition and had normal vital signs and no symptoms of infection on admission (Table 1). She had not lost any unwanted weight and had no anorexia during the last three months. The results of blood tests, ultrasound and morphological scans were completely normal. The growth chart of the pregnant mother is shown in Figure 3.
At the initial assessment, the patient had no underlying disease. Evaluation of the electronic care record in the health center showed that the patient had positive infection of COVID-19 twenty days before delivery and was treated with 200 mg of Chloroquine sulfate for 5 days.
Based on the previous history of covid-19, obstetricians requested a new PCR test for the patient, and the result was positive. IUFD was diagnosed and delivery was performed by cesarean section. Complications of labor including premature rupture of membranes, abnormal bleeding, and chorioamniotitis were not observed. After delivery, the patient was transferred to the postpartum ward and treated with antibiotics.
The newborn boy was apparently healthy but without a heartbeat. There was evidence of meconium staining of the embryonic membranes. Placenta was sent to a laboratory for pathology but IGM and IGG samples were not sent due to blood clots.
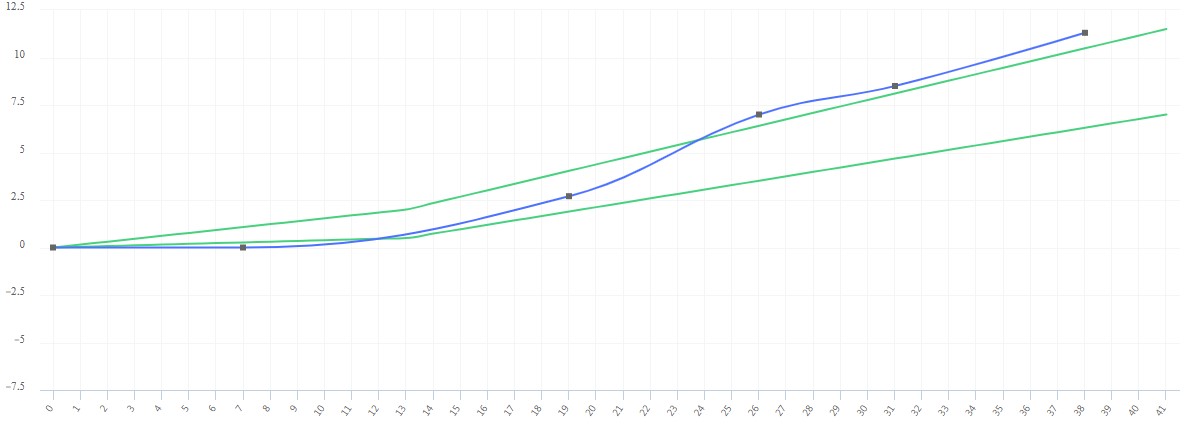
Figure 1. First pregnancy growth chart

Figure2. Second pregnancy growth chart
Figure3. Third pregnancy growth chart
Discussion
In this study all three pregnant women lived in the villages around Shahroud city, two pregnant women had a successful delivery and the neonates were born completely healthy, only one was born with diagnosis of intrauterine fetal death (IUFD) and showed Meconium Stained Amniotic Fluid (MSAF). Changes in hormone levels and the immune system function during pregnancy can make a person vulnerable to infections and serious complications. In addition, changes in fluid levels in the lungs can increase the risk of lung infections, women's lungs have more fluid during pregnancy, and increasing fluid levels put more pressure on the lungs and abdomen (11). Excess fluid stimulates the growth of bacteria and reduces the body's ability to fight infection (12). Mortality rate and complications in pregnant women are higher than in the general population (13). Shek et al., reported that the prevalence of Spontaneous abortion, premature delivery , intrauterine growth restriction, and other adverse pregnancy outcomes increased in SARS (14) . According to our study, none of the pregnant women developed severe pneumonia or died. Our findings are consistent with recent studies (1, 8, 15) and contrary to the result observed in Kayem et al., study (16). A study of 9 pregnant women with COVID-19 reported adverse outcome . These women suffered from cardiopulmonary complications in the second or third trimester of their pregnancy (17). Notably ,our observation could be affected by our small sample size and clinical characteristics and severity of infection in pregnant women who had mild pneumonia.
In the present study, one of the three pregnant women underwent vaginal delivery and two of them underwent cesarean section, because of the previous history of covid-19, and abnormal labor in the admission form. Chen et al., reported that the risk of infection transmission from pregnant woman to their neonate by vaginal delivery was the main reason for caesarean section (4). Nonetheless, to date there has been no credible evidence that cesarean delivery is a protective procedure.
Approximately 56% of intrauterine fetal deaths (IUFD) have been reported due to preeclampsia, smoking, maternal age, low birth weight, maternal hypertension and diabetes mellitus, congenital malformations and congenital anomalies (18, 19) ;and 43.7 % due to unknown causes (11).
As no convincing evidence has been found to demonstrate whether COVID-19 infection led to the intrauterine death, the cause of infant death remains unknown in this study and we are unable to ascertain a link between corona infection and IUFD.A few months ago, in Shahroud city an 18-day-old neonate was diagnosed with COVID-19 disease, and the results showed that the transmission was not vertical and was probably due to close family contact (20). In line with other studies (1, 8, 15, 21), the results of cord blood, placenta ,IgM ,IgG and neonatal throat swab samples were negative at birth and the possibility of vertical transmission from mother to newborn was ruled out. Although there is no evidence that coronavirus is transmitted to infants through breast milk(22) (21) (22) ,breast feeding has been banned for these infants due to the possibility of transmission through close contact. One of the main limitations of this study was the lack of sufficient information in the documents and the lack of careful review of cases for a long time. This study is a case report and therefore cannot draw conclusions based on the information of these people.
Conclusion
This study showed that adherence to maternal and infant care protocols ensures the health of both,but it depends on the severity of the diease in mothers. Like different effects of the virus on the general population, these effects on pregnant mothers can be different.
Acknowledgements
This work was supported by Shahroud University of Medical Sciences (Grant No. 98126).
Conflicts of Interest
The Authors declare that there is no conflict of interest.
Funding
This work was supported by Shahroud University of Medical Sciences (Grant No. 98126).
Received: 2021/02/9 | Accepted: 2021/05/16 | Published: 2022/06/30
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |