BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
URL: http://journal.zums.ac.ir/article-1-6578-en.html


 , Soheil Nasouhi1
, Soheil Nasouhi1 

 , Hoshang Bahrani2
, Hoshang Bahrani2 

 , Heydar Hosseinnejad3
, Heydar Hosseinnejad3 

 , Ehsan Akrami4
, Ehsan Akrami4 

 , Afshin Motallebzadeh5
, Afshin Motallebzadeh5 

 , Maedeh Baniasadi6
, Maedeh Baniasadi6 

 , Masoud Shahabian *7
, Masoud Shahabian *7 


2- Dept. of Anesthesiology, AJA University of Medical Sciences, Tehran, Iran
3- Dept. of Anesthesiology, Islamic Azad University, Shahrood Branch, Shahrood, Iran
4- Dept. of Pediatrics, Shahid Beheshti University of Medical Sciences, Tehran, Iran
5- Dept. of Cardiac Surgery, Razavi Hospital, Mashhad, Iran
6- Faculty of Nursing and Midwifery, Islamic Azad University, Karaj Branch, Karaj, Iran
7- Dept. of Emergency Medicine, AJA University of Medical Sciences, Tehran, Iran ,
✅ The investigation of PSA using propofol/ketamine, ketamine, and propofol/fentanyl showed similar frequencies of BIS values and adverse respiratory events. The use of propofol/fentanyl was associated with a slightly higher incidence of hypotension. Moreover, the frequency of patient satisfaction was higher among the subjects in group B, compared to those in the other groups.
Procedural sedation and analgesia (PSA) is a common clinical practice performed in the emergency department (ED) to manage pain, anxiety, and other problems patients are confronted with during medical procedures. The PSA includes the administration of sedative/dissociative medications with or without the concomitant delivery of analgesic agents. Proper sedation enhances the performance of these procedures and can lead to increased patient satisfaction (1). The patients’ rapid discharge from EDs is a key point in the expertise of ED. The clinical policy related to procedural sedation in ED varies from hospital to hospital depending on the patients’ age and conditions, sufficient equipment, and type of procedure (2). Generally, there is no ideal or standard medication for PSA. An ideal drug should cause analgesia and amnesia and induce rapid anesthesia followed by fast recovery (at the shortest possible time). Moreover, it should be expected to lack undesirable side effects. Commonly, it is required to combine an analgesic with a sedative drug. To prescribe medication, several points should be considered, including the related risks and benefits, prescription strategy, and patient’s conditions.
Various studies have investigated the different methods of general and local sedimentation. The administration should be performed with caution to prevent possible undesirable side effects. Furthermore, the choice of the appropriate method for the use of PSA drugs should be performed based on the type of procedure and patients’ conditions (3). The fastest and most reliable and predictable method is the administration of medications in the form of intravenous (IV) injection and titration of its amount to reach the proper level of sedation and analgesia. Intramuscular injection for PSA has been less frequently used in adults since it has a slower onset of action, difficult titration, and unpredictable results (4).
There are several protocols for PSA from which the most commonly used are propofol and propofol/ketamine. Propofol is suggested as a selective drug with a proper sedative and anxiolytic effect and motion/shake control for PSA in ED. The effect of propofol starts within 30 sec, and its clinical effect will be resolved within 5-7 min, and after 15 min the patient regains his consciousness (5). Propofol is commonly administered with ketamine, which acts by disconnecting the limbic and thalamocortical system leading to no linkage between the central nervous system and peripheral stimuli, such as pain. The use of ketamine leads to both relieving the pain and maintaining the stability of the cardiovascular system (6).
The bispectral index (BIS) is a modern technology for neurophysiological monitoring that continuously analyzes the patient’s electroencephalogram curve during sedation to assess the level of consciousness (3, 7, 8). Frequent monitoring of the consciousness level is recommended during PSA. The purpose of this study was to compare various PSA protocols in adults with anterior shoulder dislocation (ASD) based on the BIS in order to provide a standard method for PSA.
Study design
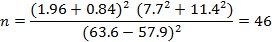
Firstly, a total of 1,432 participants were entered into this study, among whom 1,301 individuals were ineligible, while 41 subjects had unclear eligibility. Finally, 410 participants were found eligible for inclusion. Moreover, 260 cases were ineligible due to multiple trauma (n=17), abnormal vital sign (n=23), unstable to consent (n=14), unable to score (n=1), patient decline (n=53), allergy to study drugs (n=20), opium abuse (n=79), and methadone usage (n=25) (Figure 1). The patients were divided into three groups (n=50 each) based on a similar study (7).
Participants
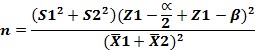
This randomized double-blinded clinical trial was conducted on 150 patients with ASD referred to the ED of Besat General Hospital in Tehran, Iran, in 2018. The sample size was determined at 46 cases in each group based on the depth of anesthesia by BIS (33) (BIS values of 63.6±7.7 and 57.9±11.4) considering the power of 80% and alpha error of 5% to detect a difference between the two groups. The sample size increased to 50 cases in each group for more accuracy using Equation 1:
Equation 1:
Inclusion and exclusion criteria
The inclusion criteria were the age range of 15-40 years, willingness for the study participation, presence of orthopedic dislocation, and normal neuromuscular examination. On the other hand, the exclusion criteria were determined as patients with underlying disease (e.g., hypertension or hypotension), diabetes, cardiac diseases, insensitivity to sedative medications, cardiovascular instability, multiple trauma, head trauma, and allergy to eggs, lecithin, and soybean seeds, as well as the presence of low oxygen saturation from the beginning of the visit, the administration of sedative and hypnotic medicines and opiates, the risk of bleeding into the abdomen or chest, and the loss of consciousness.
Procedures
All the participants had ASD and were randomly divided into three groups. The patients in groups A, B, and C were prescribed propofol/fentanyl (Caspian Tamin Company, Iran), propofol (Chemi Darou Company, Iran), and ketamine (Chemi Darou Company, Iran), respectively. In group A, the prescribed dosage was 0.5 mg/kg of propofol and 1 mcg/kg of fentanyl. In group B, the prescribed dosage was considered 1-2 mg/kg of ketamine and propofol (1:1 mixture of ketamine/propofol), and 0.75 mg/kg was infused for 10-30 sec. If a sufficient level of sedation was not observed, 0.375 mg/kg was infused again during 1-3 min to achieve the desired sedation. In addition, the prescribed dosage in group C was 1-2 mg/kg of ketamine.
Before procedures, the patients were monitored and breathed by a reservoir bag mask. The subjects were provided with facilities for the management of the advanced airway. An emergency physician who was a senior researcher conducted the procedures. To reduce the pain associated with propofol injection, a nurse gave an IV line from the antecubital vein to avoid hurting the upper limb and then injected all drugs slowly. The procedure of sedation continued to achieve sufficient depth. The BIS (33) was used for monitoring patients completely. Before the prescription (at the baseline), vital signs and the depth of sedation were measured and recorded every minute by a registered nurse up to the completion of the reduction. This process continued up to the reestablishment of clear verbal contact with the patient. After the recovery, the subjects were monitored for possible side effects. The Milch technique was used for shoulder reduction. In this technique, the subjects are placed supine after PSA, and the head of the bed is elevated 20 to 30 degrees. The affected humerus is held by the wrist and abducted gently and rotated externally. The resident stops whenever encounters resistance to motion and continues when the patient is relaxed. If the arm does not reduce while reaching 90 degrees of abduction and 90 degrees of external rotation, slow longitudinal traction is applied along the humerus while the free hand is utilized to exert lateral and superior pressure on the humeral head to complete the maneuver. The effectiveness of this method has been attributed in part to more conical symmetry of the muscle forces acting across the glenohumeral joint. A researcher-made questionnaire was completed by a registered Emergency Medicine Resident, which included induction time, procedure time, sedation time, and recovery time.
Figure 1. Consort diagram
Statistical analysis
The data analysis was conducted in SPSS software (version 23). The Chi-square test, analysis of variance, and its nonparametric equivalence were used for qualitative and quantitative analysis. P-values of less than 0.05 were considered statistically significant.
Ethical considerations
The study protocol was approved by the Ethics Committee of AJA University of Medical Sciences of Tehran, Iran (IR.AJAUMS.REC.1397.002) and registered in the Iranian Registry of Clinical Trials (IRCT20180627040258N1). According to the sampling method, the subjects were randomly assigned to three groups after thesis approval. The use of sedative drugs is morally permissible since they are routinely prescribed for PAS and their effectiveness has been demonstrated in numerous studies. The present study was performed based on the ethical principles of the Declaration of Helsinki. In line with the research ethics principles, informed consent was obtained from all the patients, and the subjects were assured of the confidentiality of their information in this study. The cases were also informed about the possibility of study withdrawal at any research stage. Moreover, the complications of each medication were explained to the participants.
Based on the obtained results of the present study, the mean values of the patients’ age and weight were obtained at 23.02±3.22 years (age range: 18-34 years) and 72.69±7.8 kg, respectively. Moreover, the mean values of visual analogue scale (VAS) scores before and after the intervention were estimated at 8.1±0.69 and 2.08±0.7, respectively. Table 1 tabulates the mean scores of age, weight, and VAS scores before and after the intervention, as well as BIS values at different times for the three groups. According to the obtained results, the comparison of VAS scores before and after the intervention showed a significant difference (Z=-10.76, P<0.005).
Table 1. Mean scores of age, weight, and VAS before and after the intervention, as well as BIS values at different times for all groups.
| Groups | Ketamine | Ketofol | Propofol/fentanyl | P-value | |||
| Mean | Standard deviation | Mean | Standard deviation | Mean | Standard deviation | ||
| Age | 23.15 | 3.18 | 23.81 | 3.86 | 22 | 2.41 | 0.44 |
| Weight | 71.11 | 9.5 | 73.42 | 6.42 | 73.1 | 7.5 | 0.9 |
| VAS before intervention | 8.08 | 0.77 | 8.18 | 0.74 | 8.2 | 0.53 | 0.68 |
| VAS after intervention | 2.18 | 0.84 | 2.04 | 0.57 | 2.04 | 0.75 | 0.67 |
| BIS before intervention | 97.42 | 1.77 | 97.7 | 1.3 | 98.7 | 1.08 | 0.9 |
| BIS at 1st min | 84.83 | 3.05 | 84.31 | 2.93 | 85.08 | 2.84 | 0.77 |
| BIS at 2nd min | 82.04 | 1.36 | 81.47 | 1.37 | 81.89 | 1.1 | 0.45 |
| BIS at 3rd min | 80.46 | 1.68 | 80.33 | 1.82 | 79.68 | 2.02 | 0.46 |
| BIS at 4th min | 77.31 | 1.7 | 77.76 | 1.33 | 77.46 | 1.56 | 0.67 |
| BIS at 5th min | 71.96 | 2.65 | 71.96 | 2.97 | 72.12 | 2.73 | 0.98 |
VAS: Visual analogue scale; BIS: Bispectral index system
Furthermore, no differences were observed between the groups in the BIS values before the intervention and at the 1st, 2nd, 3rd, 4th, and 5th min after the intervention (P<0.005). Table 2 presents the frequency rates of side effects in the patients who underwent PSA in the three groups
Table 2. Frequency of patients’ and physicians’ satisfaction for all groups.
| Variables | Ketamine | Ketofol | Propofol/fentanyl | Total | P-value | |||||
| n | % | n | % | n | % | n | % | |||
| Vomiting | No | 46 | 92 | 49 | 98 | 48 | 96 | 143 | 95.3 | 0.35 |
| Yes | 4 | 8 | 1 | 2 | 2 | 4 | 7 | 4.7 | ||
| Procedure failure | No | 0 | 0 | 0 | 0 | 0 | 0 | 149 | 99.3 | 0.36 |
| Yes | 50 | 100 | 50 | 100 | 50 | 100 | 1 | 0.7 | ||
| Agitation | No | 12 | 24 | 6 | 12 | 8 | 16 | 124 | 82.7 | 0.27 |
| Yes | 38 | 76 | 44 | 88 | 42 | 84 | 26 | 17.3 | ||
| Delusion | No | 36 | 72 | 40 | 80 | 44 | 88 | 120 | 80 | 0.22 |
| Mild | 12 | 24 | 10 | 20 | 5 | 10 | 27 | 18 | ||
| Sever | 2 | 4 | 0 | 0 | 1 | 2 | 3 | 2 | ||
| Delirium | No | 39 | 78 | 41 | 82 | 44 | 88 | 124 | 82.7 | 0.68 |
| Mild | 10 | 20 | 8 | 16 | 6 | 12 | 24 | 16 | ||
| Sever | 1 | 2 | 1 | 2 | 0 | 0 | 2 | 1.3 | ||
| Hypotension | No | 50 | 100 | 50 | 100 | 47 | 64 | 147 | 98 | 0.04 |
| Yes | 0 | 0 | 0 | 0 | 3 | 6 | 3 | 2 | ||
| Oxygen desaturation (<92) | No | 48 | 96 | 47 | 94 | 45 | 90 | 140 | 93.3 | 0.47 |
| Yes | 2 | 4 | 3 | 6 | 5 | 10 | 10 | 6.7 | ||
| Apnea | No | 48 | 96 | 49 | 98 | 50 | 100 | 147 | 98 | 0.36 |
| Yes | 2 | 4 | 1 | 2 | 0 | 0 | 3 | 2 | ||
| Respiratory rate of <8 breaths per min | No | 49 | 98 | 49 | 98 | 47 | 94 | 145 | 96.7 | 0.43 |
| Yes | 1 | 2 | 1 | 2 | 3 | 6 | 5 | 3.3 | ||
| Airway obstruction | No | 42 | 84 | 45 | 90 | 47 | 94 | 134 | 89.3 | 0.26 |
| Yes | 8 | 16 | 5 | 10 | 3 | 6 | 16 | 10.7 | ||
| Respiratory events | No | 42 | 84 | 45 | 90 | 47 | 94 | 134 | 89.3 | 0.26 |
| Yes | 8 | 16 | 5 | 10 | 3 | 6 | 16 | 10.7 | ||
In addition, the frequency of medical measurements obtained from the patients in the three groups is provided in Table 3.
Table 3. Frequency of medical measurements from the three groups.
| Variables | Ketamine | Ketofol | Propofol/fentanyl | Total | P-value | |||||
| n | % | n | % | N | % | n | % | |||
| Need for increased oxygen | No | 42 | 84 | 45 | 90 | 47 | 94 | 135 | 90 | 0.41 |
| Yes | 8 | 16 | 5 | 10 | 3 | 6 | 15 | 10 | ||
| Need for upper airway stimulation and airway repositioning | No | 47 | 94 | 48 | 96 | 49 | 98 | 144 | 96 | 0.59 |
| Yes | 3 | 6 | 2 | 4 | 1 | 2 | 6 | 4 | ||
| Need for bag and mask ventilation | No | 49 | 98 | 48 | 96 | 48 | 96 | 145 | 96.7 | 0.81 |
| Yes | 1 | 2 | 2 | 4 | 2 | 4 | 5 | 3.3 | ||
| Need for repeated dose | One | 2 | 66.7 | 4 | 50 | 6 | 75 | 12 | 63.2 | 0.74 |
| Two | 1 | 33.3 | 3 | 37.5 | 2 | 25 | 6 | 31.6 | ||
| Three | 0 | 0 | 1 | 12.5 | 0 | 0 | 1 | 5.3 | ||
Table 4 summarizes the frequency of patients’ satisfaction, physicians’ satisfaction, induction time, procedure time, sedation time, and recovery time in the three groups. According to Table 4, the comparison of the patients’ satisfaction demonstrated that there was a significant difference between the three groups (P=0.02).
Table 4. Frequency of patients’ satisfaction, physicians’ satisfaction, induction time, procedure time, sedation time, and recovery time in the three groups.
| Variables | Ketamine | Ketofol | Propofol/fentanyl | Total | P-value | |||||
| n | % | n | % | n | % | n | % | |||
| Patients’ satisfaction | Moderate | 1 | 2 | 0 | 0 | 1 | 2 | 2 | 1.3 | 0.02 |
| High | 21 | 42 | 19 | 38 | 33 | 66 | 73 | 48.7 | ||
| Very high | 28 | 56 | 31 | 62 | 16 | 32 | 75 | 50 | ||
| Physicians’ satisfaction | Moderate | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0.21 |
| High | 3 | 6 | 4 | 8 | 8 | 16 | 15 | 10 | ||
| Very high | 47 | 94 | 46 | 92 | 42 | 84 | 135 | 90 | ||
| Induction time | <2 min | 24 | 49 | 20 | 42.6 | 23 | 47.9 | 67 | 46.5 | 0.92 |
| 2-4 min | 20 | 40.8 | 20 | 42.6 | 18 | 37.5 | 54 | 40.3 | ||
| ˃4 min | 5 | 10.2 | 7 | 14.9 | 7 | 14.6 | 19 | 13.2 | ||
| Procedure time | <2 min | 26 | 52 | 33 | 66 | 24 | 48 | 83 | 55.3 | 0.43 |
| 2-4 min | 22 | 44 | 15 | 30 | 23 | 46 | 60 | 40 | ||
| ˃4 min | 2 | 4 | 2 | 4 | 3 | 6 | 7 | 4.7 | ||
| Sedation time | <5 min | 18 | 36 | 20 | 40 | 21 | 42 | 59 | 39.3 | 0.94 |
| 5-10 min | 27 | 54 | 26 | 52 | 26 | 52 | 79 | 52.7 | ||
| ˃10 min | 5 | 10 | 4 | 8 | 3 | 6 | 12 | 8 | ||
| Recovery time | <5 min | 0 | 0 | 5 | 10 | 4 | 8 | 12 | 8 | 0.87 |
| 5-10 min | 17 | 34 | 21 | 42 | 21 | 42 | 59 | 39.3 | ||
| 10-15 min | 27 | 54 | 23 | 46 | 23 | 46 | 73 | 48.7 | ||
| 15-20 min | 3 | 6 | 1 | 2 | 2 | 4 | 6 | 4 | ||
Discussion
There are many different techniques for PSA in adults with dislocated shoulder reduction. Based on the obtained results of the present study, no difference was observed regarding the outcomes, VAS scores, BIS values, physicians’ satisfaction, complications, and recovery time among the three groups.
Commonly, propofol is exclusively prescribed with an initial bolus of 1 mg/kg, and if necessary, a 0.5 mg/kg bolus is added every 3 min (9). In the present study, the need to repeat the dose was not different among the three groups. The administration of ketamine/propofol combination can decrease the dose‐dependent side effects, such as the respiratory depression of these agents. Moreover, this combination of low‐dose ketamine and propofol reduces the need to repeat medication administration (10-12). Analgesia and sedation can be produced by ketamine below the critical dosage threshold (13). However, psychomimetic reactions may occur due to a high-dose injection of ketamine (14).
The results of a study conducted by Ferguson et al., similar to the present study, indicated that no serious adverse events were observed between the propofol and ketofol groups, which introduced the administration of propofol and ketofol as similarly safe techniques for ED procedural sedation (15). Moreover, the results of another study by Andolfatto et al. showed no difference between propofol and ketofol in terms of side effects (16), which was consistent with the findings of our study.
Based on the results of the present study, no difference was observed among the three groups regarding airway obstruction and respiratory events. In a study conducted by Andolfatto et al., it was shown that the incidence of adverse respiratory events was similar in a 1:1 single-syringe combination of ketamine and propofol, as well as that of propofol and fentanyl, when targeting deep sedation (16). Moreover, a similar incidence of airway and respiratory events requiring intervention was observed in a study conducted by Ferguson et al., in which ketofol in a 1:1 ratio was compared to the equivalent volumes of 1% propofol for ED procedural sedation. According to the results of the aforementioned study, 10% of cases were reported with the need for physician’s intervention (15). In the present study, 7.3% of the patients required upper airway stimulation, airway repositioning, and bag and mask ventilation. The findings of the above-mentioned studies are consistent with those of the present study. However, an association has been shown between the incidence of respiratory adverse events with total dose and the rate of propofol administration (5, 17, 18). The high safety of ketamine provided the stability of respiratory reflexes and cardiovascular function (1, 4). The effectiveness of ketamine in the preservation of respiratory function is suggested in some studies (16, 19). It has been reported that the administration of a ketamine/propofol combination may counterbalance respiratory depression (20, 21).
Based on the findings of the present study, except for hypotension, which was observed more frequently in the propofol/fentanyl group in comparison to the ketofol and ketamine groups, no difference was observed in the incidence of other adverse events among the three groups. The results of a study carried out by Ferguson et al. revealed that hypotension was observed more frequently in the propofol group than in the ketofol group (15). The aforementioned findings may confirm the role of ketamine in preventing hypotension in patients who undergo procedural sedation. However, the results of the present study did not confirm the role of the exclusive use of propofol in causing hypotension, which was statistically similar to those of the ketofol and ketamine groups.
In the present study, BIS monitoring was performed to assess the patient’s level of consciousness. Based on the findings of a study conducted by Gan et al., the safety and efficacy of BIS monitoring were shown during propofol/alfentanil/N2O anesthesia. According to the evidence, it was demonstrated that the use of BIS could shorten the recovery time and accelerate the mother’s consciousness (22). According to the literature, it was revealed that the use of BIS reduced the administration of anesthetic drugs during the surgery (3). In addition, in another study, it was reported that routine BIS monitoring led to the decreased administration of propofol and faster recovery, in comparison to standard clinical practice (8).
In the present study, there were no differences in the BIS values before the intervention and at the 1st, 2nd, 3rd, 4th, and 5th min after the intervention. Based on the findings of a study conducted by Ferguson et al., in line with those of the present study, it was shown that the depth of sedation was similar in the propofol/fentanyl and ketofol groups (15). A minor tendency to lower sedation scores was observed in the three groups, which was consistent with the findings of other similar studies (6, 15, 16, 23). In the case of using an agent with analgesic properties and one without these characteristics, the sedation depth is increased with the analgesic agent.
In the study conducted by Ferguson et al., a higher rate of intraprocedural compliance was observed in patients who underwent ketofol therapy in comparison to those in the propofol group; however, the rate of agitation was reported to be lower during ketofol therapy (15). This finding was confirmed by the results of a study by Andolfatto et al. (16), nevertheless, rejected by those of a study by Miner et al. (6). It has been reported that the rate of unpleasant emergence due to the administration of ketofol is lower than the exclusive usage of ketamine (24). Ketamine can increase thalamic sensory output and arousal, and the arousal characteristic of ketamine may control the sedative effects of propofol. This can be explained as the dose‐dependent interaction of these agents (25).
In the present study, the comparison of VAS scores before and after the intervention showed no significant difference between the three groups. Generally, ketofol is effective for ED procedural sedation, and there is no difference in the outcomes of patients using ketofol and propofol (6, 16, 23). Although the results of the present study were in line with those of other studies, some methodological differences, such as the application of oxygen and opiate, were observed between them. On the other hand, in a similar study conducted by Ferguson et al., a lower pain score was reported in the ketofol group 30 min following the procedure, in comparison to that in the propofol group. Moreover, the frequency of patients’ satisfaction was higher among the subjects in the ketofol group (62%) than in the other groups. Ferguson et al. reported high satisfaction in propofol and ketefol groups; nonetheless, no difference was observed between the groups. These discrepancies in the results may be attributed to some differences in the sample size and used dosage between the aforementioned study and the present study.
In a study carried out by Wathen et al., ketamine was compared to ketamine/midazolam combination (26), the findings of which showed no difference in the recovery agitation between the groups. According to the results of a study conducted by Sener et al., the comparison of the side effects of ketamine and ketamine/midazolam combination in adults indicated a lower rate of recovery agitation in the ketamine group (27). Considering the concerns regarding the role of ketamine administration in the emergence phenomena in adults (reported at 10-20% in the literature), it is commonly used with caution (28). It is recommended to carry out future studies in this regard.
In the present study, delirium was observed in all groups with a minor frequency. The emergence of delirium was slightly higher in the ketofol group, in comparison to the other groups; nevertheless, there was no significant difference regarding this. Similarly, the findings of the study by Ferguson et al. showed the existence of an association between some degree of delirium emergence and administration of both propofol and ketofol. In the mentioned study, a more severe emergence of delirium was seen in the ketofol group, which was in line with the results of the present study (15). The duration in which a resuscitation bed is occupied is important in a busy ED. Waiting time and prolonged time spent in ED are among the main problems in ED (29). The use of PSA elongates the hospital stay, thereby increasing the duration of patient’s monitoring. Both accurate follow-up and continued monitoring of the patient require a longer hospital stay and lead to greater responsibility in ED (2).
The investigation of the collected data of the present study revealed no difference in the recovery time among the three groups. Based on the results of the study conducted by Ferguson et al., the recovery time was shorter in the propofol group than in the ketofol group (15). Regarding the comparison of ketamine and midazolam/fentanyl, Jamal et al. reported lower complications and faster recovery in the ketamine group (30). The reason for these discrepancies may be the differences in the sample size, patient’s demographic characteristics, eligible criteria, methods of measuring variables, as well as the type of administered drugs and their dosage. According to the evidence, the comparison of intra-articular lidocaine injection with IV propofol and pethidine showed that the length of admission in ED and duration of the procedure from the beginning of local infusion were significantly higher in the propofol group, compared to the other groups. Overall, the intra-articular injection is recommended in cases with dislocation intervals of less than 5 h, while the IV injection method is suggested for other cases (31).
Generally, there is still no major agreement among physicians on the selection of a preferred method regarding the protocol and type of analgesic and pain reliever medications. The success of any technique depends on the physician’s skills and choice of the appropriate anesthetic method (32).
Advantages and limitations
One of the main limitations of this study was associated with high sample attrition due to inconsistency with eligible criteria. To alleviate this problem, the sample size was selected larger than what was determined by the formula.
Conclusion
The investigation of PSA using propofol/ketamine, ketamine, and propofol/fentanyl showed similar frequencies of BIS values and adverse respiratory events. The administration of propofol/fentanyl was associated with a slightly higher incidence of hypotension. Moreover, the frequency of patients’ satisfaction was higher among the subjects in the propofol-ketamine group than in the other groups.
Acknowledgements
This paper was extracted from a thesis submitted for the partial fulfillment of requirements for the emergency medicine residency program at AJA University of Medical Sciences in Tehran, Iran. A part of these results has already been presented in the conference "14th Iranian Annual Congress of Emergency Medicine" (history 1 October 2019, Country: Iran) in the acknowledgment section. Hereby, the authors would like to extend their gratitude to all the staff working in the Emergency Department of Besat General Hospital for the approval of the project proposal. The authors also wish to thank Zamen Publishing Company and Ms. Mitra Golmohammadi for the statistical analysis of the present study.
Conflicts of Interest
The authors declare that there is no conflict of interest.
Received: 2021/06/9 | Accepted: 2022/07/7 | Published: 2022/08/8
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |