BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
URL: http://journal.zums.ac.ir/article-1-6678-en.html
2- Dept. of Occupational Therapy, School of Allied Medical Sciences, Zanjan University of Medical Sciences, Zanjan, Iran
3- Rehabilitation Research Center, Iran University of Medical Sciences (IUMS), Tehran, Iran ,
4- Dept. of Occupational Therapy, School of Rehabilitation Sciences, Iran University of Medical Sciences, Tehran, Iran
✅ As psychometric data proved inconsistency and conflict for the majority of studies, only provisional judgments may be established. Psychometric features for assessment instruments are clearly partial or lacking, limiting rationale for use in clinical settings or research until more psychometric information is provided.
The phenomenon of aging, with all psychological, social, cultural, religious, and economic aspects, is a serious and challenging issue for families and societies in developed and developing countries. According to literature, one-third of the community will be 65 or older by the year 2050 (1). Additionally, in Iran, the elderly population will increase by 33% over the next 35 years (2). Consequently, the rapid growth of this age group has also made the diagnosis, treatment, and prevention of their problems very essential (3).
In older adults, fear of falling (FOF) is acknowledged as a significant psychological component (4). Bandura points out that psychological factors, like self-efficacy, are related to falling, in addition to physical and physiological factors (5). According to literature, FOF is very common among older adults, and is reported to have a prevalence of 25% to 92% (6-8). FOF may have consequences like limitations in mobility, social alienation, depression, anxiety, and poor quality of life (8-10). Also, neural and musculoskeletal systems that underlie balance weaken as people age. This deterioration leads to an increased probability of falling. On the other hand, home environmental hazards as extrinsic physical factors, cause about 40% of falls. Due to the aforementioned consequences on individuals, researchers have developed various tools for evaluating psychological and physical aspects of falling (11).
These psychological and physical aspects are important in clinical trials of fall prevention. Nursing care professionals, geriatricians, and rehabilitation specialists need to have a clear understanding of a range of measures to provide detailed strategies and interventions. The best way to select an outcome measure is by choosing one with superior psychometric properties. Outcome measures must be valid (i.e., measures the construct specifically), reliable (i.e., produce similar results under unchanged conditions), and responsive (i.e., detect clinically important changes as time passes) (12).
In the past years, a substantial number of outcome measures were developed and validated all over the world. Previous systematic reviews have evaluated only physical or psychological aspects of falling in older adults (11,13-15). An examination of which outcome measures are validated in Persian older adults and which is more comprehensive and useful is essential for future research and clinical practice. An overview of these studies is lacking; hence, this COSMIN systematic review was carried out to review psychometric features of psychological and physical fall outcome measures in Persian older adults.
Search strategy and terms
This COSMIN systematic review was conducted according to the Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) guidelines (16). Literature search was done using the following databases from 1971 to June 2021: PubMed, Scopus, Medline, CINAHL, PsychINFO, ProQuest, Cochrane library, Web of Science, Pedro, SID, CIVILICA, Magiran, MEDLIB, IranDoc, and IranMedex. Terwee and coworkers’ COSMIN recommendation search strategy and filters were employed (17). The databases were searched using Medical Subject Heading (MeSH) terms: “accidental falls”, “falls”, “falling”, “slip and fall”, “aged”, “geriatrics”, “frail elderly”, “aging”, “geriatric assessment”, “patient-reported outcome measures”, “patient outcome assessment”, “self-assessment”, “self-report”, “reproducibility of results”, “validation studies”, “validation studies as a topic”, and “psychometrics” coupled with the following phrases: “fall-related psychological outcomes”, “consequence of falls”, “fear of falling”, “concern about falling”, “worry about falling”, “falls self-efficacy”, “afraid of falling”, “balance”, “balance confidence”, “aging”, , “older adults”, “elderly”, “elders”, “old people”, “community-dwelling”, “independent living”, “reliability”, “validity”, “responsiveness”, “Persian”, “Farsi”, and “Iran*”. A further hand search of the extracted articles’ bibliographic references was carried out to identify potential studies that were not captured in electronic databases. The search included grey literature discovered by Google Scholar in order to access all relevant publications.
Study selection and data extraction
The search procedure was performed by two investigators (P.M. and M.Z.). After removing duplicates by Endnote X7 software, the titles and abstracts of the retrieved articles were inspected by two independent reviewers (M.M. and P.M.) to assess eligibility. Articles were deemed eligible if: 1) the article was about assessment tools in psychological and physical fall assessment tool in older adults; 2) full-text was accessible; 3) involvement of participants aged 65 or over. Articles were excluded if they were about the assessment of psychological or physical aspects of fall for other age groups and diseases such as Alzheimer’s, Multiple sclerosis, Parkinson’s, cancer, heart disease, vestibular disorders, and amputation. Articles free of exclusion were reviewed and disagreements were resolved through consensus conferences. If no consensus could be reached, the third reviewer made the final decision (A.A.).
Methodological quality
The risk of bias checklist from the COnsensus-based Standards for the Selection of Health Measurement INstruments (COSMIN) was used to evaluate the methodological quality of the included publications (12). First, each study was appraised as very good, adequate, doubtful, or inadequate quality. Second, the results of each study were graded as (+) sufficient, (₋) insufficient, or (?) indeterminate. Third, using the GRADE (Grading of Recommendations Assessment, Development, and Evaluation) approach, the cumulative evidence for each measurement tool was summarized and appraised. Based on this approach, each evidence was contemplated to be of high quality. However, based on the risk of bias, inconsistency, imprecision, and indirectness, the quality would be reduced by one or two levels to moderate, low, or very low (18). Two reviewers independently appraised the methodological quality and psychometric results of the listed research (M.M. and P.M.). When there was disagreement, a debate with the third reviewer resulted in a consensus (A.A.).
The PRISMA flowchart for the research included in this review is depicted in Figure 1 (5). Of the initial 1268 studies, 33 studies met the inclusion criteria. In this regard, 8 and 12 assessment tools for psychological and physical aspects of falling were validated in Persian older adults, respectively. Table 1 shows the general features of various assessment tools.
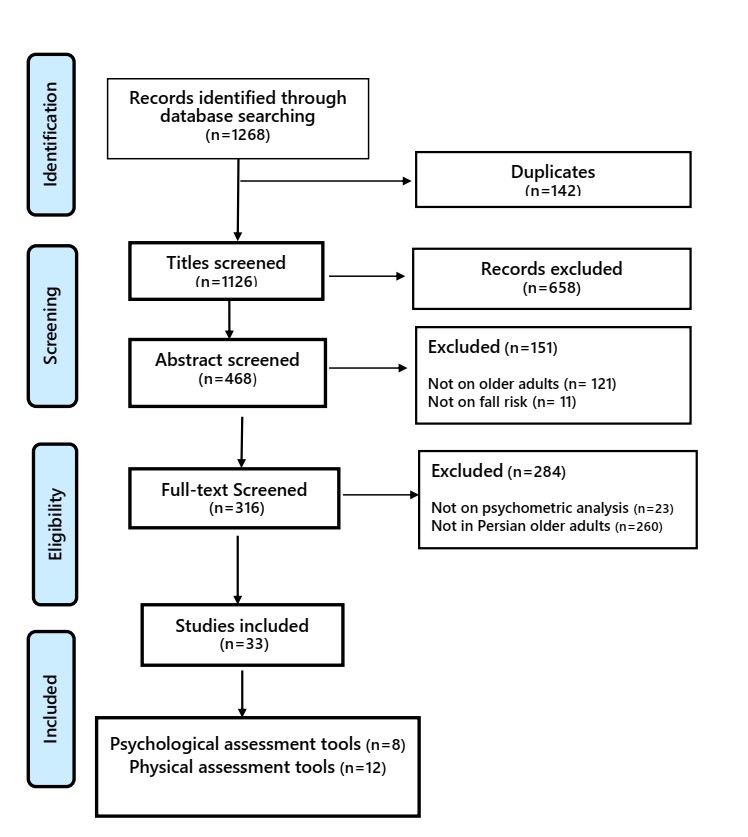
Figure 1. PRISMA flowchart of studies reported in this systematic review
General characteristics of psychological assessment tools
Fall Efficacy Scale (FES): This scale was designed to examine the level of perceived efficacy in 10 basic daily activities. Higher scores indicate FOF in older adults. This scale is used for providing information for goal-setting, as well as monitoring changes in intervention. Due to inclusion of a limited range of everyday activities, the FES is more suitable for frail older persons. Furthermore, the FES is appropriate for screening older people without cognitive decline (19). On the other hand, fall concerns in active and high-functioning older adults cannot be captured accurately by this scale (2, 20-22).
modified Falls Efficacy Scale (mFES): The mFES is a 14-item modified version of the FES. The mFES includes outdoor activities, which the FES does not cover. Therefore, this scale can be used in active community-dwelling older people. Unlike the FES, higher scores indicate more confidence (23).
Falls Efficacy Scale- International (FES-I): This scale was developed with 16 items (10 items from the original FES and 6 added items regarding more physically and socially demanding activities) due to the criticisms on the original FES. This scale can be used in both self-report and interview formats. The FES-I is regarded as a criterion in literature. The downsides of the FES-I are as follows: 1) more items can cause fatigue in older adults; 2) difficulty in administration due to time constraints in crowded clinical settings (24, 25).
Short version of Falls Efficacy Scale-International (Short FES-I): This short scale is comprised of 7 extracted items from the 16-item FES-I. These items cover indoor, outdoor, and social activities. Lower scores on this scale reflect better self-efficacy (26).
Activities-specific Balance Confidence scale (ABC): This scale is designed to assess balance confidence in a wide range of indoor and outdoor activities. Participants are asked to rate their balance confidence from 0% (not confident) to 100% (complete confidence) in 16 balance-demanding activities. The summation divided by 16 represents the final score (22, 27-29).
Fear of Falling Avoidance Behavior Questionnaire (FFABQ): This questionnaire was designed by Landers et al., (2011) to assess avoidance in certain activities due to FOF. This self-report questionnaire consists of 14 activities. Higher scores indicate more avoidance and restriction in activities (30).
Geriatric Fear of Falling Measure (GFFM): This 15-item screening tool was developed to assess perceptions about falls and conditions when FOF develops among older adults in Taiwan. This scale is divided into three subscales: psychosomatic symptoms (4 items), risk prevention attitude (5 items), and modifying behavior (6 items). The merits of this measure are items that entail action and ratings that are not hypothetical (31).
modified Gait Efficacy Scale (mGES): This self-report scale was developed to assess confidence and ability in 10 walking scenarios. Items are graded on a scale from 1 (no
Table 1. General features of fall-related psychological and physical assessment tools for Persian older adults
| Assessment tools | Items | Scoring | Construct measured | Available versions |
| Falls Efficacy Scale (FES) |
10 | 1-10 Total score:10-100 |
Psychological | English, Swedish, Serbian, Korean, Persian |
| modified Falls Efficacy Scale (mFES) |
14 | 0-10 Total score:0-140 |
Psychological | Chinese, French, Gujarati, Hindi, Turkish, English, Spanish, Serbian, Bahasa, Swedish, Igbo, Persian |
| Falls Efficacy Scale-International (FES-I) |
16 | 1-4 Total score:16-64 |
Psychological | Greek, Italian, Spanish, Turkish, German, Dutch, Chinese, Portuguese, Swedish, Arabic, Norwegian, English, Filipino, Persian |
| Short version of Falls Efficacy Scale-International (Short FES-I) | 7 | 1-4 Total score:7-28 |
Psychological | English, Mandarin, Bahasa Malaysia, Portuguese, Chinese, Dutch, Italian, Japanese, Persian |
| Activities-specific Balance Confidence Scale (ABC) | 16 | 0-100% Total score: summation divided by 16 |
Psychological | English, Chinese, Italian, Hebrew, German, Korean, Dutch, Hindi, Portuguese, Spanish, Swedish, Turkish, Persian |
| Fear of Falling Avoidance Behavior Questionnaire (FFABQ) | 14 | 0-4 Total score:0-56 |
Psychological | English, Turkish, Korean, Persian |
| Geriatric Fear of Falling Measure (GFFM) |
15 | 1-5 Total score:15-75 |
Psychological | English, Persian |
| modified Gait Efficacy Scale (mGES) |
10 | 1-10 Total score:10-100 |
Psychological | Portuguese, Chinese, Japanese, Dutch, German, English, Persian |
| Home Falls and Accident Screening Tool (HOME FAST) (Self-report [SR] and Health Professional [HP] formats) |
SR:87 HP:25 |
0-1 Total score:0-25 |
Physical | English, Portuguese, Chinese, Korean, Persian |
| Johns Hopkins Fall Risk Assessment Tool (JHFRAT) | 8 aspects | Different scoring for each aspect Total score:0-35 |
Physical | English, Spanish, Chinese, Portuguese, Korean, Persian |
| Performance-Oriented Mobility Assessment (POMA) | 16 | 2- or 3- point Total score:0-28 |
Physical | English, Portuguese, Turkish, German, Korean, Persian |
| Berg Balance Scale (BBS) |
14 | 0-4 Total score:0-56 |
Physical | Portuguese, French, Arabic, German, Greek, Italian, Japanese, Korean, Norwegian, Swedish, Turkish, Spanish, Persian |
| Short Berg Balance Scale (BBS-9) |
9 | 0-4 Total score:0-36 |
Physical | English, Persian |
| Timed Up and Go (TUG) |
3 sequences | Time (seconds) | Physical | English, Chinese, Portuguese, Persian |
| Fullerton Advanced Balance Scale (FAB Scale) |
10 | 0-4 Total score:0-40 |
Physical | English, German, Korean, Turkish, Persian |
| Dynamic Gait Index (DGI) |
8 | 0-3 Total score:0-24 |
Physical | Arabic, Danish, Finnish, Korean, Portuguese, English, Persian |
| Functional Gait Assessment (FGA) |
10 | 0-3 Total score:0-30 |
Physical | Portuguese, German, Korean, Swedish, English, Persian |
| Functional Reach Test (FRT) |
1 sequence | Distance (centimeter) | Physical | All languages* |
| Brief Balance Evaluation System Test (Brief-BES Test) |
14 | 0-3 Total score:0-24 |
Physical | English, Turkish, Japanese, Persian |
| Gait Speed | 1 | Time (seconds) | Physical | All languages* |
Note: * Due to the performance-based nature of these assessment tools, these are available for all languages
confidence) to 10 (complete confidence), providing a total score between 10 to 100 (32).
General characteristics of physical assessment tools
Home Falls and Accident Screening Tool (HOME FAST): This screening tool was designed to identify older people who may experience fall owing to environmental and functional factors. This tool is available in self-report (SR) and health professional (HP) formats. The HOME FAST-HP consists of 25 items. Each item is rated dichotomously (hazard present, no hazard). The HOME FAST-SR consists of 87 items with a dichotomous “Yes” or “No” rating scale. The total score in the SR format is calculated based on a conversion table of the HOME FAST-HP (33-35).
Johns Hopkins Fall Risk Assessment Tool (JHFRAT): The JHFRAT evaluates fall risk in eight aspects: age (1 to 3 points), fall history (5 points), elimination (2 to 4 points), medication (3 to 7 points), patient care equipment (1 to 3 points), mobility (2 points), and cognition (1 to 4 points). Scores ≤6, 7-13, ≥14 indicate low, moderate, and high fall risk in older adults, respectively (36).
Performance-oriented Mobility Assessment (POMA): This assessment tool evaluates fall risk related to balance and gait abilities in older people. The POMA comprises two subscales: Balance subscale: 9 items, Gait subscale: 7 items. A total score of <19, 19-24, and >24 reflect low, moderate, and high fall risk, respectively (37,38).
Berg Balance Scale (BBS): The BBS evaluates fall risk and static balance in functional tasks with 14 items. The BBS has been considered as the gold standard; however, its ceiling effect causes older adults with mild balance impairments under-identified (39-42).
Short Berg Balance Scale (BBS-9): The BBS-9 assesses functional balance in high-functioning older adults with 9 items driven from the original BBS. Scoring is similar to the original BBS, but the highest total score is 36. Scores lower than 32 indicate fall risk in older people (43).
Timed Up and Go (TUG): The TUG measures mobility, balance, and fall risk in older people. The time taken to stand up from a chair, walk 3 meters, turn around and return to the chair, and sitting down is recorded (44-46).
Fullerton Advanced Balance Scale (FAB Scale): This scale is designed to identify subtle fluctuations in balance among high-functioning elderly. This scale consists of 10 performance-based tasks. Higher scores indicate better balance performance (41, 47, 48).
Dynamic Gait Index (DGI): The DGI was designed to evaluate dynamic postural stability in older adults. The DGI has 8 items with a 4-point scoring. Higher scores reflect better performance (49, 50).
Functional Gait Assessment (FGA): The FGA reflects balance and gait abilities by 7 items from the DGI and 3 additional items. This assessment can be conducted on a walkway with a 6-meter length and 30-centimeter width (41, 44, 51).
Functional Reach Test (FRT): The FRT is a quick measure of equilibrium in older people. It is measured as the highest distance one can reach forward beyond normal arm length, sustaining a static base of support in standing. The FRT measures stability during self-initiated movements and stability limits. It has been widely used to assess balance in various diseases worldwide (45).
Brief Balance Evaluation System Test (Brief-BES Test): This test evaluates balance with 6 items, which are from each subsection of the full BESTest (52).
Gait Speed: The gait speed is measured by walking at a comfortable speed with shoes over a 10-meter distance. The distance is determined by a tape on the floor to mark the start and endpoint. Additional tapes are pasted 2-meters before and after the course to control acceleration and deceleration. The time in the middle 10-meters is recorded by a stopwatch (44).
Methodological quality of the assessment tools
The constructs studied were structural validity, internal consistency, and hypothesis testing that were based on reliable methodology with superb quality. In contrast, content validity was either doubtful or not reported. Neither of the studies that were included examined cross-cultural adaptation and responsiveness. Methodological quality and psychometric properties of the Persian studies for each tool are reported in Tables 2 and 3, respectively.
Table 2. Methodological quality of the studies conducted on measurement tools
| Instrument | Study | Validity | Reliability | Measurement error | Responsiveness | |||||
| Content | Structural | Hypothesis testing | Cross-cultural adaptation | Criterion | Internal consistency | Reliability | ||||
| FES | Dadgari et al., (2015) (39) | Doubtful | NR | NR | NR | NR | Very good | NR | NR | NR |
| Fadavi-Ghaffari et al., (2019) (2) | Doubtful | Adequate | Very good | NR | NR | Very good | Adequate | Very good | NR | |
| Meimandi et al., (2020) (19) | NR | NR | NR | NR | Very good | NR | NR | NR | NR | |
| mFES | Mosallanezhad et al., (2011) (23) | NR | NR | Moderate | NR | NR | Very good | Adequate | Very good | NR |
| FES-I | Baharlouei et al., (2013) (25) | Doubtful | NR | Very good | NR | NR | Very good | Adequate | NR | NR |
| Khajavi (2013) (24) | NR | Adequate | NR | NR | NR | Very good | Doubtful | NR | NR | |
| Short FES-I | Kashani (2019) (26) | Doubtful | Very good | Very good | NR | NR | Very good | Adequate | NR | NR |
| ABC | Hassan et al., (2015) (27) | NR | NR | NR | NR | NR | Very good | Adequate | NR | NR |
| Khajavi (2017) (29) | NR | Adequate | NR | NR | NR | Very good | Adequate | NR | NR | |
| Dadgari et al., (2015) (39) | Doubtful | NR | NR | NR | NR | Very good | NR | NR | NR | |
| Kashani (2018) (43) | NR | Very good | Very good | NR | NR | Very good | Adequate | NR | NR | |
| FFABQ | Heidarian (2020) (30) | Doubtful | Very good | Very good | NR | NR | Very good | Adequate | NR | NR |
| GFFM | Sadeghi (2021) (31) | Doubtful | NR | Very good | NR | NR | Very good | NR | NR | NR |
| mGES | Khajavi et al., (2017) (32) | NR | Adequate | Very good | NR | NR | Very good | Adequate | NR | NR |
| HOME FAST | Maghfouri et al., (2012) (35) | NR | NR | NR | NR | NR | Doubtful | Adequate | NR | NR |
| Maghfouri et al., (2013) (34) | Doubtful | NR | NR | NR | NR | NR | Adequate | Adequate | NR | |
| Karimi et al., (2019) (33) | Doubtful | NR | Very good | NR | NR | NR | Adequate | Very good | NR | |
| JHFRAT | Hojati et al., (2018) (36) | Doubtful | NR | NR | NR | NR | Very good | NR | NR | NR |
| POMA | Jahantabinejad et al., (2018) (38) | NR | NR | NR | NR | Very good | NR | NR | NR | NR |
| Moulodi et al., (2020) (37) | NR | Inadequate | Very good | NR | NR | Very good | Adequate | Very good | NR | |
| BBS | Kamrani et al., (2003) (42) | NR | NR | NR | NR | Inadequate | NR | NR | NR | NR |
| Salavati et al., (2012) (40) | NR | NR | Very good | NR | NR | Inadequate | Adequate | NR | NR | |
| Dadgari et al., (2015) (39) | NR | NR | NR | NR | NR | Inadequate | NR | NR | NR | |
| Pourmahmoudian et al., (2020) (41) | NR | NR | NR | NR | NR | Very good | NR | NR | NR | |
| BBS-9 | Kashani et al., (2018) (28) | Doubtful | Very good | NR | NR | NR | Very good | NR | NR | NR |
| TUG | Kamrani et al., (2010) (44) | NR | NR | Very good | NR | NR | NR | NR | NR | NR |
| Azadi et al., (2014) (46) | NR | NR | NR | NR | NR | NR | Adequate | Very good | NR | |
| Aslankhani et al., (2015) (45) | NR | NR | Very good | NR | Inadequate | Very good | Adequate | NR | NR | |
| FAB Scale | Sabet et al., (2016) (48) | NR | NR | Very good | NR | NR | Very good | Adequate | Very good | NR |
| Azad et al., (2020) (47) | Doubtful | Very good | Very good | NR | Inadequate | Very good | Adequate | Very good | NR | |
| Pourmahmoudian et al., (2020) (41) | NR | NR | NR | NR | Very good | NR | NR | NR | NR | |
| DGI | Abdiani et al., (2014) (49) | NR | Adequate | Very good | NR | NR | Very good | Inadequate | NR | NR |
| Abdiani et al., (2015) (50) | NR | Adequate | Very good | NR | NR | Very good | Doubtful | NR | NR | |
| FGA | Kamrani et al., (2010) (44) | NR | Adequate | Very good | NR | NR | NR | NR | NR | NR |
| Kamrani et al., (2010) (51) | NR | NR | Very good | NR | NR | NR | NR | NR | NR | |
| Pourmahmoudian et al., (2020) (41) | NR | NR | NR | NR | Very good | NR | NR | NR | NR | |
| FRT | Aslankhani et al., (2015) (45) | NR | NR | Very good | NR | Inadequate | NR | Adequate | NR | NR |
| Brief-BESTest | Kashani et al., (2019) (52) | NR | Very good | NR | NR | NR | Very good | NR | NR | NR |
| Gait Speed | Kamrani et al., (2010) (44) | NR | NR | Very good | NR | NR | NR | NR | NR | NR |
Note: ABC: Activities-specific Balance Confidence Scale; BBS: Berg Balance Scale; BBS-9: Short Berg Balance Scale; Brief-BES Test: Brief Balance Evaluation System Test; DGI: Dynamic Gait Index; FAB Scale: Fullerton Advanced Balance Scale; FES: Falls Efficacy Scale; FES-I: Falls Efficacy Scale-International; FFABQ: Fear of Falling Avoidance Behavior Questionnaire; FGA: Functional Gait Assessment; FRT: Functional Reach Test; GFFM: Geriatric Fear of Falling Measure; HOME FAST: Home Falls and Accident Screening Tool; JHFRAT: Johns Hopkins Fall Risk Assessment Tool; mFES: modified Falls Efficacy Scale; mGES: modified Gait Efficacy Scale; POMA: Performance-Oriented Mobility Assessment; Short FES-I: Short version of Falls Efficacy Scale-International; TUG: Timed Up and Go; NR: Not Reported
Table 3. Methodological quality of the assessment tools
| Instrument | Study | Content Validity |
Structural Validity |
Hypothesis testing | Criterion Validity | Internal Consistency | Reliability | Measurement Error |
| FES | Dadgari et al., (2015) (39) |
Not enough information | NR | NR | NR | α=0.89 | NR | NR |
| Fadavi-Ghaffari et al., (2019) (2) |
Not enough information | KMO:0.92 2 factors |
Strong to high correlation with FES-I and SIQ (ρ:0.72-0.92, P<0.001) |
NR | α=0.95 | ICC=0.98 | SEM=2.16 MDC=11.23 |
|
| Meimandi et al., (2020) (19) |
NR | NR | NR | AUC:0.91 S:81%- 100% Sp:90%-100% |
NR | NR | NR | |
| mFES | Mosallanezhad et al., (2011) (23) |
NR | NR | Low to moderate correlations (r=-0.26-0.57) |
NR | α=0.75 | ICC=0.99 | SEM=1.82 |
| FES-I | Baharlouei et al., (2013) (25) |
Not enough information | NR | Significant weak to strong correlations (r=-0.33-0.60) |
NR | α=0.92-0.93 | ICC=0.79-0.94 Total:0.87 |
NR |
| Khajavi (2013) (24) |
NR | KMO:0.96 1 factor |
NR | NR | α=0.98 | r=0.70 | NR | |
| Short FES-I | Kashani (2019) (43) |
Not enough information | CFI: 1; TLI: 1 GFI:0.98; RMSEA:0.02 |
Acceptable correlation with FES-I (r=0.74) |
NR | α=0.95 | ICC=0.87 | NR |
| ABC | Hassan et al., (2015) (27) |
NR | NR | NR | NR | α=0.96 | ICC=0.97 | NR |
| Khajavi (2017) (29) |
NR | KMO:0.95 1 factor |
NR | NR | α=0.98 | Gutman:0.95 ICC=0.85; r=0.82 |
NR | |
| Dadgari et al., (2015) (39) |
Not enough information | NR | NR | NR | α=0.89 | NR | NR | |
| Kashani (2018) (28) |
NR | CFI, GFI, TLI:0.99 RMSEA:0.08 |
With ABC-6 (r=0.93) | NR | α=0.97 | ICC=0.83 | NR | |
| FFABQ | Heidarian (2020) (30) |
Not enough information | KMO:0.82 1 factor |
Moderate to high (r=0.64-0.77) | NR | α=0.97 | ICC=0.97 | NR |
| GFFM | Sadeghi (2021) (31) |
Not enough information | NR | High correlation with ABC (r=-0.79) | NR | α=0.75-0.89 | NR | NR |
| mGES | Khajavi et al., (2017) (32) |
NR | KMO: 0.93 1 factor |
Strong correlation with FES-I (r=-0.93) and ABC (r=0.95) |
NR | α=0.97 | r=0.91-0.96 Total:0.96 |
NR |
| HOME FAST | Maghfouri et al., (2012) (35) |
NR | NR | NR | NR | >0.8 for all items | Kappa coefficient: 0.65-1.00 | NR NR |
| Maghfouri et al., (2013) (34) |
Not enough information | NR | NR | NR | NR | ICC=0.72 ICC=0.88 |
SEM=0.54 SEM=0.84 |
|
| Karimi et al., (2019) (33) |
Not enough information | NR | Strong correlation with health professional format (ρ=0.95, P<0.001) | NR | NR | ICC=0.99 | SEM=0.25 | |
| JHFRAT | Hojati et al., (2018) (36) |
Not enough information | NR | NR | NR | α=0.73 | NR | NR |
| POMA | Jahantabinejad et al., (2018) (38) |
NR | NR | NR | AUC:0.91 S:86%; SP 86% |
NR | NR | NR |
| Moulodi et al., (2020) (37) |
NR | RMSEA:0.12, TLI:0.8 AGFI:0.68, GFI:0.76 CFI:0.85, NFI:0.83 2 factors |
With BBS (r= 0.85-0.90), FAB (r= 0.77-0.85), DGI (r= 0.79-0.82), TUG (r= -0.73-0.75), gait speed (0.63-0.66), step length (r= 0.34-0.42), step test (r= 0.65-0.68) | NR | Balance: α=0.91 Gait: α=0.84 Total: α=0.94 |
ICC=0.95-0.97 ICC=0.90-0.92 |
SEM=0.81-1.05 MDC=1.48-2.91 SEM=0.86-1.72 MDC=2.38-4.76 |
|
| BBS | Akbari Kamrani et al., (2003) (42) |
NR | NR | NR | S:88.24%; SP:89.19% |
NR | NR | NR |
| Salavati et al., (2012) (40) |
NR | NR | High and negative correlation with TUG: (r=-0.74, P<0.001) | NR | α=0.62 | ICC=0.93 ICC=0.95 |
NR | |
| Dadgari et al., (2015) (39) |
NR | NR | NR | S:63%; SP:97% | NR | NR | NR | |
| Pourmahmoudian et al., (2020) (41) |
NR | NR | NR | AUC:0.75 S:61%; SP:92% |
NR | NR | NR | |
| BBS-9 | Kashani et al., (2018) (43) |
Not enough information | RMSEA:0.08, GFI:0.91 TLI:0.97, CFI:0.98 |
NR | NR | α=0.90 | NR | NR |
| TUG | Akbari Kamrani et al., (2010) (44) |
NR | NR | Moderate to strong (r=0.58-0.81) | NR | NR | NR | NR |
| Azadi et al., (2014) (46) |
NR | NR | NR | NR | NR | ICC=0.64-0.82 | SEM=0.97-2.25 MDC=1.91-4.42 |
|
| Aslankhani et al., (2015) (45) |
NR | NR | Moderate and negative correlation with BBS (r=-0.64, P<0.0001) | S:78% SP:23% |
α=0.81 | ICC=0.98 | NR | |
| FAB Scale | Sabet et al., (2016) (48) |
NR | NR | Moderate to strong correlation with BBS, TUG, FRT (ρ= 0.62-0.77) | NR | α=0.83-0.84 | ICC=0.98 Kappa coefficient: 0.63-1.00 |
SEM=0.17 MDC=0.46 |
| Azad et al., (2020) (47) |
Not enough information | RMSEA:0.05, NFI:0.92 CFI:0.92, TLI:0.91 AGFI:0.92, GFI:0.91 |
Low to moderate correlation with BBS, TUG, FRT (r=0.44-0.77) | S:81.25% SP:52.78% |
α=0.83 | ICC=0.92 Kappa coefficient: 0.72-1.00 |
SEM=1.25 MDC=3.46 |
|
| Pourmahmoudian et al., (2020) (41) |
NR | NR | NR | AUC:0.76 S:58%, Sp:86% |
NR | NR | NR | |
| DGI | Abdiani et al., (2014) |
NR | KMO:0.94 1 factor |
Divergent validity: U:1009, P<0.0001 | NR | α=0.95 | r=0.79 ICC or weighted kappa NR |
NR |
| Abdiani et al., (2015) (49) |
NR | KMO:0.87 1 factor |
Divergent validity: U:1035, P<0.0001 | NR | α=0.89 | r=0.71-0.87 | NR | |
| FGA | Kamrani et al., (2010) (51) |
NR | KMO:0.87 2 factors |
Divergent validity: t:14.81, P<0.001 | NR | NR | NR | NR |
| Kamrani et al., (2010) (44) |
NR | NR | Moderate to high correlation with TUG, gait speed, number of fall (r=-0.70-0.81) Divergent validity: t:-6.73, P<0.001 |
NR | NR | NR | NR | |
| Pourmahmoudian et al., (2020) (41) |
NR | NR | NR | AUC:0.79 S:63%, Sp:76% |
NR | NR | NR | |
| FRT | Aslankhani et al., (2015) (45) |
NR | NR | Moderate correlation with BBS (r=0.79) | S:80%, Sp:21% | NR | ICC=0.97 | NR |
| Brief-BESTest | Kashani et al., (2019) |
NR | RMSEA:0.02, GFI:0.97 CFI:1.00, TLI:1.00 |
NR | NR | α=0.88 | NR | NR |
| Gait Speed | Kamrani et al., (2010) (51) |
NR | NR | Moderate to high correlation with TUG, gait speed, number of fall (r=0.64-0.77) |
NR | NR | NR | NR |
Note: ABC: Activities-specific Balance Confidence Scale; BBS: Berg Balance Scale; BBS-9: Short Berg Balance Scale; Brief-BESTest: Brief Balance Evaluation System Test; DGI: Dynamic Gait Index; FAB Scale: Fullerton Advanced Balance Scale; FES: Falls Efficacy Scale; FES-I: Falls Efficacy Scale-International; FFABQ: Fear of Falling Avoidance Behavior Questionnaire; FGA: Functional Gait Assessment; FRT: Functional Reach Test; GFFM: Geriatric Fear of Falling Measure; HOME FAST: Home Falls and Accident Screening Tool; JHFRAT: Johns Hopkins Fall Risk Assessment Tool; mFES: modified Falls Efficacy Scale; mGES: modified Gait Efficacy Scale; POMA: Performance-Oriented Mobility Assessment; SIQ: Single Item Question; Short FES-I: Short version of Falls Efficacy Scale-International; TUG: Timed Up and Go; NR: Not Reported
Overall quality of the studies
As shown in Table 4, there is a broad range of discrepancies (from high to low) in the overall quality of each measurement tool’s psychometric features. The Brief-BESTest and gait speed had consistently high results (44, 52). The mGES, mFES and FGA are the only measures with consistent and moderate to high results (23, 32, 41, 44, 51).
Table 4. General quality of the evidence for each assessment tool
| Instrument | Validity | Reliability | Measurement error | Responsiveness | |||||
| Content | Structural | Hypothesis testing | Cross-cultural adaptation | Criterion | Internal consistency | Reliability | |||
| FES | Low (±) | Moderate (±) | High (+) | NR | High (+) | High (+) | Moderate (±) | High (+) | NR |
| mFES | NR | NR | Moderate (±) | NR | NR | High (+) | Moderate (±) | High (+) | NR |
| FES-I | Low (±) | Moderate (±) | High (+) | NR | NR | High (+) | Low (±) | NR | NR |
| Short FES-I | Low (±) | High (+) | High (+) | NR | NR | High (+) | Moderate (±) | NR | NR |
| ABC | Low (±) | Moderate (±) | High (+) | NR | NR | High (+) | Moderate (±) | NR | NR |
| FFABQ | Low (±) | High (+) | High (+) | NR | NR | High (+) | Moderate (±) | NR | NR |
| GFFM | Low (±) | NR | High (+) | NR | NR | High (+) | NR | NR | NR |
| mGES | NR | Moderate (±) | High (+) | NR | NR | High (+) | Moderate (±) | NR | NR |
| HOME FAST | Low (±) | NR | High (+) | NR | NR | Low (±) | Moderate (±) | Moderate (±) | NR |
| JHFRAT | Low (±) | NR | NR | NR | NR | High (+) | NR | NR | NR |
| POMA | NR | Low (±) | High (+) | NR | High (+) | High (+) | Moderate (±) | High (+) | NR |
| BBS | NR | NR | High (+) | NR | Low (±) | Moderate (±) | Moderate (±) | NR | NR |
| BBS-9 | Low (±) | High (+) | NR | NR | NR | High (+) | NR | NR | NR |
| TUG | NR | NR | High (+) | NR | Low (±) | High (+) | Moderate (±) | High (+) | NR |
| FAB Scale | Low (±) | High (+) | High (+) | NR | Moderate (±) | High (+) | Moderate (±) | High (+) | NR |
| DGI | NR | Moderate (±) | High (+) | NR | NR | High (+) | Low (±) | NR | NR |
| FGA | NR | Moderate (±) | High (+) | NR | High (+) | NR | NR | NR | NR |
| FRT | NR | NR | High (+) | NR | Low (±) | NR | Moderate (±) | NR | NR |
| Brief-BES Test | NR | High (+) | NR | NR | NR | High (+) | NR | NR | NR |
| Gait Speed | NR | NR | High (+) | NR | NR | NR | NR | NR | NR |
Note: ABC: Activities-specific Balance Confidence Scale; BBS: Berg Balance Scale; BBS-9: Short Berg Balance Scale; Brief-BES Test: Brief Balance Evaluation System Test; DGI: Dynamic Gait Index; FAB Scale: Fullerton Advanced Balance Scale; FES: Falls Efficacy Scale; FES-I: Falls Efficacy Scale-International; FFABQ: Fear of Falling Avoidance Behavior Questionnaire; FGA: Functional Gait Assessment; FRT: Functional Reach Test; GFFM: Geriatric Fear of Falling Measure; HOME FAST: Home Falls and Accident Screening Tool; JHFRAT: Johns Hopkins Fall Risk Assessment Tool; mFES: modified Falls Efficacy Scale; mGES: modified Gait Efficacy Scale; POMA: Performance-Oriented Mobility Assessment; SIQ: Single Item Question; Short FES-I: Short version of Falls Efficacy Scale-International; TUG: Timed Up and Go; NR: Not Reported
Discussion
When the overall quality ratings for each psychometric property per measurement are summed, it is obvious that many psychometric features are incomplete or absent, restricting their usage in clinical settings or research until further psychometric details are available. However, more investigation on the following neglected psychometric characteristics is urgently needed: content validity, criterion validity, measurement error, and responsiveness. The scarcity of psychometric information for these measures in literature is problematic. When no evidence on psychometric attributes is provided, no conclusions on the assessment’s properties may be established. Limited data on psychometric attributes may not always suggest poor psychometric quality; nevertheless, it does indicate that the evaluation was chosen and employed in clinical practice or research without sufficient psychometric proof. For instance, if responsiveness is uncertain, utilizing it as an outcome measure in research raises serious issues regarding the generalization of the results because there is no proof that the measurement can detect change over time. Poor ability to detect change (i.e. responsiveness), may produce false-negative results on the effect of therapy. Furthermore, content validity is regarded as the most important aspect of an instrument. If no proof of content validity is supplied, the assessment’s content will be under question. Consequently, interpretation and generalizability of the findings will be affected. Clinicians should not only evaluate aim and features of a test, but also the quality of psychometric properties should be in mind.
Assessments with high-quality for all psychometric elements should be preferred over those with no or low-quality. Further research on content validity, measurement error, criterion validity, responsiveness, and cross-cultural validity is required to allow practitioners and researchers to make evidence-based decisions in geriatric rehabilitation. Following COSMIN and PRISMA guidelines, the present study was the first review of fall risk measures in Persian older adults. Additionally, the results were analyzed rigorously based on the COSMIN risk of bias checklist. The study limitation is that we did not evaluate interpretability since the COSMIN framework does not consider it a psychometric quality (12).
Implications for rehabilitation
Conclusion
Performance-based and physical assessment tools are dependent on culture. However, Psychological constructs of falls cannot be captured objectively. Therefore, we recommend that rather than a single assessment tool, two or more assessment tools with psychological and physical constructs be used in combination to maximize rehabilitation outcomes.
Acknowledgements
The authors are grateful to the researchers who provided additional information about instruments.
Ethical consideration
Approval was obtained from the research ethics board of the Iran University of Medical Sciences (IR.IUMS.REC.1398.1189).
Conflicts of Interest
The authors declare that they have no competing interests.
Received: 2021/08/23 | Accepted: 2022/06/20 | Published: 2022/08/8
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |