BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
URL: http://journal.zums.ac.ir/article-1-6855-en.html
2- Dept. of Operating Room, School of Paramedicine, Hamadan University of Medical Sciences, Hamadan, Iran ,
3- Dept. of Surgery, Clinical Research Development Unit, Peymanieh Hospital, Jahrom University of Medical Sciences, Jahrom, Iran
4- Modeling of Non-Communicable Disease Research Center, Hamadan University of Medical Sciences, Hamadan, Iran
✅ Based on these findings, low pressure of pneumoperitoneum with active evacuation compared to the standard pressure, efficiently reduced shoulder pain intensity. Thus, using low-pressure pneumoperitoneum in laparoscopic cholecystectomy is recommended to relieve postoperative pain.
Technique and minimally invasive surgical procedure for removing gallbladder in patients (1) and for treating cholecystitis (acute/chronic), symptomatic cholecystitis, biliary dyskinesia, acute cholecystitis, gallstone pancreatitis and masses (2).Today,approximately 93% of cholecystectomy surgeries are performed laparoscopically (3).Laparoscopic cholecystectomy has mainly replaced open cholecystectomy (4) and has high satisfaction regarding high vision, the minimum operating time, and anesthesia for the patient and the surgeon (5).
Laparoscopic cholecystectomy has advantages over open cholecystectomies, such as shorter hospitalization,faster discharge and recovery, less pain, better aesthetic results, and lower mortality rates (6, 7), but several patients have complained about hemodynamic, metabolic, humoral, and neurological changes in addition to changes in the levels of serum liver enzymes after surgery (8, 9).
Although the pain severity following laparoscopic cholecystectomy is generally lower compared to the open method, it is important to note that some patients may still experience abdominal and shoulder pain for several days after the laparoscopic procedure (10). Postoperative shoulder pain has been reported in a range of 35% to 80% of cases, with some instances lasting for more than 72 hours following surgery (11-13).
Shoulder pain is an irritating symptom that delays postoperative recovery (14). Factors causing shoulder pain include the stimulation of the sympathetic neurons by an increase in carbon dioxide (15) and the persistence of carbon dioxide in the peritoneal cavity (16).
The hypothesized mechanism for shoulder pain is the diaphragm stretching due to the rate of blowing carbon dioxide (10), and the diaphragm is stimulated by the acidity of the peritoneal fluid induced by carbonic acid (17). In other words, pain occurs in the scapula through stimulating the phrenic nerve, which originates from the third and fifth cervical nerves (C3-C5) and controls movement and provides sensation in the diaphragm (18).
Residual carbon dioxide gas also causes decreased intraoperative urinary output, decreased respiratory compliance and cardiac output, and decreased venous blood flow (19, 20).
According to the evidence, various methods such as suctioning the remaining gas in the abdominal cavity (21), using the transverse abdominal muscle (22), reducing the pressure of gas blown in the abdomen (23), using Anti-inflammatory drugs (24), local anesthesia of the diaphragm (25) and local anesthesia of the peritoneal surface in the surgical incision area (26) have been used to reduce the occurrence of shoulder pain after laparoscopic cholecystectomy.
International guidelines recommend that to minimize the effect of pneumoperitoneum on normal physiology and the positive effect on postoperative pain, the lowest intra-abdominal pressure that causes adequate surgical exposure should be used instead of routine pressure (27). Low pneumoperitoneum pressure is defined as a pressure ranging from 6-10 mm Hg (28). The main concern with low-pressure pneumoperitoneum is the immunity against inadequate exposure, which leads to longer operating times than usual, increased intraoperative complications, and increased chance of turning into open, laparoscopic procedures (29).
Studies have shown that using low pressure during pneumoperitoneum is related to better tolerance during surgery and postoperative recovery and reducing surgical pain severity (11). Previous studies have been performed mainly on patients with standard carbon dioxide pressure surgery. Since studies have yielded mixed results, researchers have not reached a consensus on using low-pressure carbon dioxide and abdominal suctioning at the end of the procedure. Therefore, this study investigated how the standard pressure and low-pressure pneumoperitoneum with active evacuation affect shoulder pain intensity in patients with laparoscopic cholecystectomy.
Study Design
This research involved a prospective clinical trial study, registered under the code IRCT20210502051161N1, conducted in 2021 on patients undergoing laparoscopic cholecystectomy at Ostad Motahhari Hospital in Jahrom, south of Iran. The sample size was estimated using Equation 1. With a 95% confidence interval and a 90% power level, the minimum required number for each group was 36 patients, which increased to 40 patients in each group, considering a 10% drop. Thus, in total, 80 patients were recruited using convenience sampling.
Inclusion Criteria
The survey included the participation of patients aged between 18 and 70 years, who underwent elective laparoscopic cholecystectomy, had an ASA class I or II, no history of drug addiction or intense analgesia usage, no administration of anti-anxiety medication, and provided informed consent.
Exclusion Criteria
The following criteria were considered as exclusion criteria in this survey: pregnancy and lactation, a history of major abdominal surgery, ASA class 3 and above, long-term use of nonsteroidal anti-inflammatory drugs, coagulation problems, conversion from laparoscopic to open surgery, referral to the intensive care unit, and severe complications such as bleeding and shock.
Study Instruments
Data were collected using questionnaires regarding patients’ information (demographics) and background and the visual rating scale (VAS). The demographic characteristics included questions about age, gender, level of education, occupation, marital status, body mass index (BMI), history of surgery, and time of CO2 surgery.
Pain severity was evaluated using the VAS scale. This scale is a 10-cm linear index ranging from 0 (no pain) to 10 (most severe pain). Patients were asked to mark the 10-cm line on the numbers better describes their degree of pain. Then, using a ruler, the distance from this point to the beginning point of zero was measured, and the number was considered the patient’s pain. This scale is the most reliable pain rating system widely used in pain-related research. The validity and reliability of this scale were 94% and 97%, respectively (30).
Intervention Process
After receiving a referral letter from Jahrom University of Medical Sciences, the researcher came to visit the patients on the day of surgery according to the list of people ready for laparoscopic cholecystectomy surgery, transferred patients to the operating room unit, and after introducing himself, completed the demographic information of all patients.
Patients in the intervention and control groups did not know about the type of intervention to be performed after entering the operating room. The same method was used for anesthesia in both groups. General anesthesia was started with midazolam and sufentanil as premedication or before anesthesia. Propofol and atracurium were used to induce anesthesia, and isoflurane, intravenous propofol, and morphine were used to continue anesthesia.
After anesthesia, three ports were used for the surgery in both groups. A direct trocar, which is embedded under the navel, was used to perform pneumoperitoneum. The pneumoperitoneum pressure for blowing carbon dioxide gas in both groups was initially set at the standard level of 14-15 mm Hg. In the intervention group, the pressure was adjusted to 8-11 mm Hg after entering all three trocar ports. However, in the control group, the pressure remained unchanged.
In the intervention group, the operation site was suctioned for two minutes after and at the end of the procedure, following gallbladder removal. However, in the control group, no such action was taken. The trocars were removed, and the skin was sutured. Patients were transferred to the recovery room after regaining consciousness. After leaving the operating room and transferring to the surgical ward, patients were evaluated by the VAS scale after 2, 6, 12, and 24 hours of surgery in both groups. Due to the severity of patients’ pain and the need for analgesic drugs, they have prescribed analgesics (like pethidine) to relieve their pain following the operation for three intervals (6, 12, and 24 hours later).
Data Analysis
Statistical analysis was performed with SPSS software version 21. The normality distribution of the data in the study groups was assessed using the Shapiro-Wilk test. Mann-Whitney test was used to compare the pain severity between groups, and the Friedman test was used to compare pain severity within the group. The significance level used in this study was set at 0.05.
Ethical Approval
This research was approved by the ethics committee of Hamadan University of Medical Sciences (with the ethical code of IR.UMSHA.REC.1400.131). The objectives and method of the study were explained to every patient, together with obtaining an informed consent document to assure them about the confidentiality of the information.
This study compared the effect of the standard pressure with low-pressure pneumoperitoneum and active evacuation on shoulder pain intensity in patients with laparoscopic cholecystectomy. Tables 1 and 2 compare demographic characteristics in the intervention and control groups.
Table 1. The frequency of qualitative demographic variables in patients based on the intervention and control groups
| Variables | Frequency | ||
| Control Group | Intervention Group | ||
| Gender | Man | 6 (15%) | 8 (20%) |
| Woman | 34 (85%) | 32 (80%) | |
| Education | Illiterate | 8 (20%) | 4 (10%) |
| Elementary | 11 (27.5%) | 7 (17.5%) | |
| Middle School | 2 (5%) | 7 (17.5%) | |
| Diploma | 14 (35%) | 14 (35%) | |
| University Degree | 5 (12.5%) | 8 (20%) | |
| Marital Status | Single | 5 (12.5%) | 8 (20%) |
| Married | 35 (87.5%) | 32 (80%) | |
| Job | Employee | 1 (2.5%) | 4 (10%) |
| Worker | 3 (7.5%) | 1 (2.5%) | |
| Free Job | 5 (12.5%) | 3 (7.5%) | |
| Retired | 2 (5%) | 5 (12.5%) | |
| Householder | 29 (72.5%) | 27 (67.5%) | |
| History of Surgery | Yes | 24 (60%) | 27 (67.5%) |
| No | 16 (40%) | 13 (32.5%) | |
Table 2. The frequency of quantitative demographic variables in patients based on the intervention and control groups
| Variables | Mean ± St.D | |
| Control Group | Intervention Group | |
| Age | 43.55 ± 13.32 | 40.98 ± 9.40 |
| BMI | 26.33 ± 5.15 | 25.97 ± 3.08 |
| CO2 Use | 91.26 ± 40.70 | 107.75 ± 42.75 |
| Pneumoperitoneum Time (min) | 35.25 ± 9.47 | 42.0 ± 6.88 |
According to the results, the mean age of patients in the control and intervention groups was 43.55 ± 13.32 and 40.98 ± 9.40, respectively. Most of them were married women (34 (85%) in the control and 32 (80%) in the intervention groups) and had a diploma (14 (35%) in both groups). Demographic characteristics and contextual variables were comparable and identical in both groups (Table 1). No deaths, bile duct injuries, or open surgery were observed in the groups. There were also no changes from low pressure to standard pressure pneumoperitoneum.
The frequency of post-surgical shoulder pain was assessed; the results are indicated in Table 3.
Table 3. The frequency of shoulder pain in intervention and control groups at different time intervals after the surgery
| Time | VAS Score (0-10) | Frequency | P-value | |
| Control Group | Intervention Group | |||
| 2 Hours | 0 | 20 (50.0%) | 30 (75.0%) | 0.053 |
| 1 | 11 (27.5%) | 7 (17.5%) | ||
| 2 | 9 (22.5%) | 3 (7.5%) | ||
| 6 Hours | 0 | 1 (2.5%) | 2 (5.0%) | 0.093 |
| 1 | 8 (20%) | 18 (45.0%) | ||
| 2 | 20 (50.0%) | 16 (40.0%) | ||
| 3 | 9 (22.5%) | 3 (7.5%) | ||
| 4 | 2 (5.0%) | 1 (2.5%) | ||
| 12 Hours | 1 | 4 (10.0%) | 5 (12.5%) | 0.048 |
| 2 | 13 (32.5%) | 22 (55.0%) | ||
| 3 | 22 (55.0%) | 10 (25.0%) | ||
| 4 | 1 (2.5%) | 3 (7.5%) | ||
| 24 Hours | 0 | 2 (5.0%) | 8 (20%) | 0.001 |
| 1 | 24 (60.0%) | 30 (75.0%) | ||
| 2 | 12 (30.0%) | 2 (5.0%) | ||
| 3 | 2 (5.0%) | 0 (0.0%) | ||
Accordingly, 25 and 50 percent of the cases in the intervention and control group had experienced shoulder pain two hours after the operation. Also, the frequency of pain in grades 1 and 2 was less in the intervention group compared to the control group. After 6, 12, and 24 hours from the operation, most of the patients in the intervention and control groups had experienced shoulder pain, but the difference in the shoulder pain between the intervention and control groups was significant after 12 hours (P = 0.048) and 24 hours (P = 0.001) from the surgery (Table 3).
The shoulder pain intensity after the surgery was compared between the intervention and control groups; the results are indicated in Table 4 and Figure 1.
Table 4. The intensity of shoulder pain in intervention and control groups after the surgery
| Shoulder Pain In VAS | Time (h) | P-Value (Within Groups)* |
||||
| 2 | 6 | 12 | 24 | |||
| Control Group | Median | 0.50 | 2 | 3 | 1.00 | 0.001 |
| IQR+ | 1-0 | 3-2 | 3-2 | 2-1 | ||
| Intervention Group | Median | 0 | 1.50 | 2 | 1.00 | 0.001 |
| IQR | 0.5-0 | 2-1 | 3-2 | 1-1 | ||
| P-Value (Between Groups)** |
0.016 | 0.006 | 0.094 | 0.001 | ||
* Friedman test
** Mann-Whitney test
+ Interquartile range
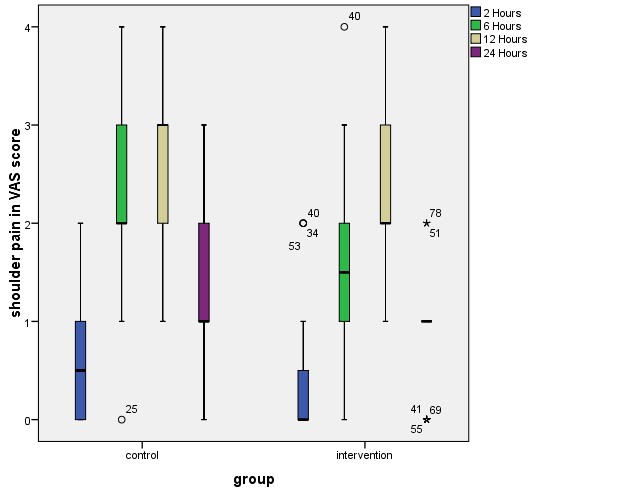
Figure 1. The intensity of shoulder pain after surgery in the intervention and control groups
The intragroup comparison revealed that the median pain intensity in both the intervention and control groups initially increased from 2 hours after surgery to 12 hours after surgery, followed by a subsequent decrease. However, it is worth noting that the median shoulder pain severity, as measured by the VAS score, in the intervention group was significantly higher than the control group after 2, 6, and 24 hours post-surgery (Table 4 and Figure 1). Pethidine was prescribed at different doses to relieve moderate to severe post-operation pain after different hours of the surgery. The frequency of prescribed pethidine is compared between the intervention and control groups, and the results are shown in Table 5.
Table 5. The amount of pethidine used in the intervention and control groups
| Time (h) | Pethidine Dose (mg) | Frequency of Prescriptions | P-value | |
| Control Group | Intervention Group | |||
| 6 | 0.0 (none) | 10 (25%) | 25 (62.5%) | 0.144 |
| 25.00 | 26 (65%) | 14 (35%) | ||
| 50.00 | 4 (10%) | 1 (2.5 %) | ||
| 12 | 0.0 (none) | 36 (90%) | 39 (97.5%) | 0.169 |
| 25.00 | 4 (10%) | 1 (2.5%) | ||
| 50.00 | - | - | ||
| 24 | 0.0 (none) | 40 (100%) | 40 (100%) | - |
| 25.00 | - | - | ||
| 50.00 | - | - | ||
In both the intervention and control groups, pethidine with a dose of 25 mg was administered 2 and 12 hours after the surgery. However, 6 hours after the surgery, a higher dosage of 50 mg was prescribed for four patients in the control group and one in the intervention group. Although less pethidine was prescribed in the intervention group compared to the control group, there was no significant difference between the used pethidine in the intervention and control groups (P > 0.05).
Based on the results, it can be implied that low-pressure pneumoperitoneum and active evacuation reduced the intensity of postoperative shoulder pain so that the pain incidence rate was lower in the intervention group than in the control group. The common dose of pethidine was 25 mg, but 6 hours after the surgery, 50 mg was used for some patients.
Discussion
It can be said that laparoscopic cholecystectomy as a standard treatment for gallbladder diseases is related to reduced complications and decreased pain. Although the mechanism of pain caused by low-pressure pneumoperitoneum is unknown, it is hypothesized that peritoneal stimulation causes pain due to excessive bloating and stretching of the abdominal and peritoneal muscles by pneumoperitoneum CO2 (31).
Numerous studies have sought to minimize the duration of pain and recovery following laparoscopic cholecystectomy; however, they have yielded varying outcomes and findings. As in the present study, through meta-analysis of randomized trials and previous studies, the beneficial effects of low-pressure pneumoperitoneum on postoperative shoulder pain have been demonstrated (13, 32, 33).
Tripathi et al. (2020) and Neogi et al. (2020) reported the use of low-pressure pneumoperitoneum to reduce hemodynamic changes compared to the standard pressure and suggested a safer method for gallbladder laparoscopy (11, 13). In the study of Neogi et al. (2020), laparoscopic pneumoperitoneum patients were divided into two groups: low-pressure and standard-pressure. The occurrence and intensity of postoperative shoulder pain at 2, 8, 24, and 48 hours in the standard-pressure group were significantly higher than in the low-pressure pneumoperitoneum group (11). In the study conducted by Tripathi et al. (2020), patients undergoing laparoscopic cholecystectomy were divided into two groups: the low-pressure pneumoperitoneum group and the standard-pressure pneumoperitoneum group (13).
In another study, Rajnish et al. (2017) considered using lavage serum at the end of laparoscopic gallbladder surgery in the peritoneal cavity to reduce shoulder pain effectively. However, in this study, the pressure used for pneumoperitoneum was not reported (33).
A review of the evidence showed that shoulder pain appears 2-6 hours after surgery and gradually increases in severity to about 12 hours and then begins to decrease (32), which is consistent with the results of the present study. Some studies have reported the severity of shoulder pain at 8 and 24 hours after surgery (34). In general, studies such as the present study have shown a delay in the onset of shoulder pain. It is important to note that in the present study, the patients of both groups had similar and relatively short operating times (an average of 35 minutes in the control group and 39 minutes in the intervention group). The duration of low-pressure pneumoperitoneum surgery typically takes two minutes longer than the standard procedure, but the clinical relevance of this difference is unclear (35). This short operation time may justify a shorter period of shoulder pain (5, 34).
Residual pneumoperitoneum volume also affects shoulder pain after laparoscopic cholecystectomy (5). Sabzi et al. (2014) measured the residual volume of pneumoperitoneum by chest X-ray 24 hours after laparoscopic cholecystectomy and reported very high abdominal and shoulder pain in patients with moderate to severe residual gas volume. In the present study, although the residual volume of pneumoperitoneum was not measured, its protocol was the same as the study of Sabzi et al. for the complete removal of intra-abdominal gas (5).
However, certain findings have presented contradictory outcomes. As Chang et al. (2021) did not show any difference in postoperative pain at different pressures of pneumoperitoneum during laparoscopic cholecystectomy and recommended the routine use of low-pressure pneumoperitoneum only in patients who needed low-pressure pneumoperitoneum surgery (36). Their study was performed in three groups of pneumoperitoneum with the standard pressure reduction (12-14 mm Hg), low-pressure pneumoperitoneum (9-11 mm Hg), and very low-pressure pneumoperitoneum (6-8 mm Hg) (36).
The reason can be attributed to different causes of pain after laparoscopic cholecystectomy (37). Patient characteristics, underlying disease, wound site, low-pressure pneumoperitoneum, and cholecystectomy site may be present, and preoperative and postoperative distorting factors may also affect pain levels. On the other hand, perforation of the gallbladder during bile leakage may irritate the peritoneum, and placement of the drainage tube may cause pain.
It is important to note that although the present study showed that low-pressure pneumoperitoneum and active evacuation are effective in relieving shoulder pain, and although the surgeon for low-pressure pneumoperitoneal surgery has reduced vision and longer time of operation, its benefits, such as reduction of postoperative pain, reduction of analgesia, and reduction of hospital stay are noteworthy (38). This method is notably safe if managed by an experienced surgeon, but the surgeon’s comfort level at normal pressure is undoubtedly better than at low pressure (11).
One of the limitations of this study was that since the culture and pain tolerance threshold in various groups of people is different, these factors may affect the research findings. The Visual Pain Scale (VAS) has eliminated this problem.
Conclusion
According to the present study, low-pressure pneumoperitoneum and active evacuation effectively reduce shoulder pain in patients undergoing laparoscopic cholecystectomy compared to the standard pressure. Therefore, it is recommended to routinely utilize low-pressure pneumoperitoneum to alleviate postoperative pain following laparoscopic cholecystectomy. On the other hand, due to the difficulty of the low pneumoperitoneum for the surgeon compared to the standard pressure, it seems that there is a need for more studies on the physical and mental state of the surgeons in long-term surgeries. On the other hand, it is suggested to perform interventions with different pneumoperitoneal pressures in patients undergoing laparoscopic cholecystectomy in future studies.
Acknowledgements
This study has been derived from an MSc. thesis funded by the Vice-chancellor for Research and Technology, Hamadan University of Medical Sciences (No.140002071015).
Conflicts of Interest
The authors declare no conflict of interest.
Received: 2022/09/16 | Accepted: 2023/03/26 | Published: 2023/06/26
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |






