BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
URL: http://journal.zums.ac.ir/article-1-7076-en.html
2- Dept. of Internal Medicine, School of Medicine, Rafsanjan University of Medical Sciences, Rafsanjan, Iran
✅ We report the case of a 45-year-old woman who presented with recurrent episodes of acute pancreatitis. Appropriate diagnostic and therapeutic interventions should be undertaken for primary hyperparathyroidism to prevent the recurrence of pancreatitis and hypercalcemia.
Primary hyperparathyroidism (PHPT) is caused by increased parathyroid hormone (PTH) secretion due to single parathyroid adenoma, multiple adenomas, hyperplasia, carcinoma, etc. (1). Increased PTH can cause hypercalcemia (2). On the other hand, hypercalcemia can result in acute pancreatitis (AP) and is associated with worse outcomes of AP (3,4), but presentation of PHPT with both hypercalcemia and acute pancreatitis is rare, which only a few cases have been reported as hypercalcemic pancreatitis caused by PHPT itself (5-7). Here, we report a case of PTH which presented with recurrent acute pancreatitis and hypercalcemia crisis.
The patient, a 45-year-old woman, was referred to the Emergency Department (ED) of Ali Ibn AbiTaleb Hospital in Rafsanjan, Iran. She complained of epigastric pain, which had a sudden onset, accompanied by nausea and vomiting for a day. The pain also radiated to her back. Notably, the patient had experienced the same conditions six months prior. Her medical history revealed a diagnosis of deep vein thrombosis (DVT) five years ago (without a specific reason) and acute pancreatitis six months earlier (with an average serum calcium level but without a specific reason). There were no records of other disorders, and she denied any history of drug, cigarette, opioid, or alcohol consumption. Additionally, the patient had no relevant allergies or adverse family medical history.
Physical Examination Upon Admission
Upon admission, the patient was conscious, oriented, and cooperative. Her vital signs (temperature, blood pressure, heart rate, respiratory rate, and O2 saturation) were within normal range. However, she presented with signs of mild dehydration. Mild epigastric tenderness was detected during the abdominal examination, but no rebound tenderness. Bowel sounds were typical and heard within two minutes. Examinations of other systems, including cardiopulmonary, neurological, and musculoskeletal, were unremarkable.
Laboratory Examinations
The patient's laboratory examinations on admission yielded the following results: White blood cell count; 2.71 × 109/L (within the reference range of 4-10 × 109/L) with (94.9% neutrophils) hemoglobin, 125.0 g/L; PLT count, 461 × 109/L; Gamma glutamic-pyruvic transaminase, 10.7 mg/dl; alkaline phosphatase, 282 µ/L; urea,12.2 mmol/L; creatinine, 0.82 mg/dl; and TSH, 0.81 Uiu/ML Furthermore, the following markers were assessed to evaluate pancreatitis: serum amylase 850 µ/L; serum sodium, 142 mmol/L; serum potassium, 3 mmol/L; serum calcium, 13.3 mmol/ L; serum Albumin, 3.8 g/dL.
Subsequently, due to the high calcium level, a serum PTH level test was conducted, which revealed a value of 158.8 pmol/L, leading to the consideration of a diagnosis of PHPT for this patient. A 24-hour urine test also resulted in 1200 ml/24h for volume, 576 mg/24h for creatinine, and 400 mg/ 24h for calcium.
Imaging Examinations
Abdominal ultrasonography showed no abnormalities in the gallbladder or pancreas, and the neck ultrasound revealed no lesions.
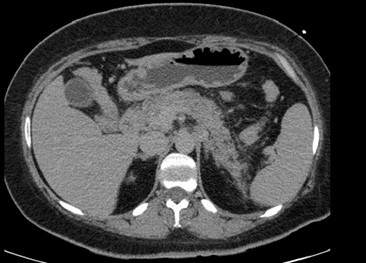
Abdominal computed tomography revealed peri-pancreatic fat without contusion and exudative changes around the pancreas. There were also no signs of gallbladder, biliary system, or stone abnormalities. Therefore, the patient was diagnosed with acute pancreatitis (Figure 1).
Figure 1. Abdomen computed tomography revealed peri-pancreatic fat with no contusion, exudative changes around the pancreas.
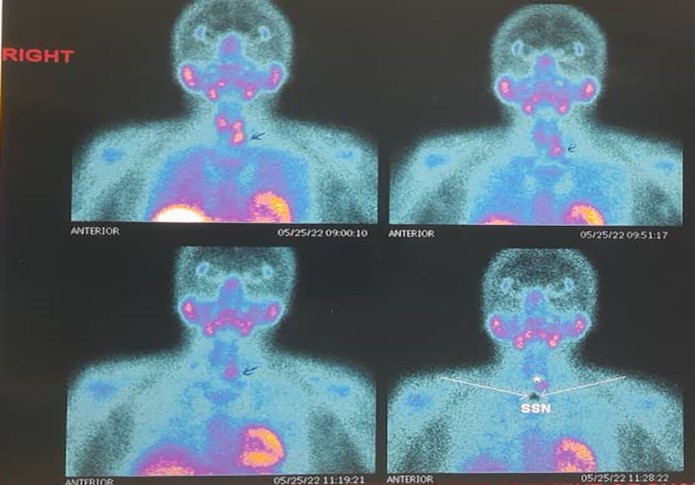
Electrocardiography and echocardiography showed no abnormalities Further Diagnostic Workup. The patient was referred to Kerman for a Sestamibi scan, which revealed a parathyroid adenoma (Figure 2).
Figure 2. Sestamibi scan, which revealed parathyroid adenoma
Final Diagnosis
Based on her clinical manifestations, biochemical parameters, and para-clinic findings, she was diagnosed with primary hyperparathyroidism (PHPT) combined with acute pancreatitis and hypercalcemia.
Treatment
The patient received hydration with approximately three liters of normal saline serum daily during the admission. Additionally, 90 mg pamidronate ampoules were infused over two hours with cardiac monitoring, and calcitonin was administered at 200 units Q8h to address the high serum calcium concentration.
Considering the high risk of cardiovascular and cerebrovascular events and the worsening condition of the patient's pancreatitis, the surgery option was discussed with the patient and her family. They accepted the recommendation, and the patient was considered a candidate for parathyroidectomy.
Finally, the surgery pathology results confirmed the presence of a parathyroid adenoma with a water-clear cell pattern in the left inferior parathyroid gland.
The patient was discharged and followed up for one year after the operation. The patient fully recovered during this period, and her serum PTH and calcium levels remained normal. Furthermore, she showed no symptoms of pancreatitis.
Discussion
PTHP is a common endocrine disorder that results from an increased level of serum PTH hormone and presents with changes in some serum biomarkers levels, including increased serum calcium, reduced serum phosphate, increased, standard, and rarely decreased urinary calcium; increased urinary phosphate; increased serum chlorine; hypergammaglobulinemia; and increased serum alkaline phosphatase (1).
PHPT has three common predominant phenotypes: symptomatic, asymptomatic, and normocalcemic (8). Although the serum calcium level can be expected in PHPT (known as Normocalcemic PHPT), hypercalcemia is the most common biochemical hallmark of PHPT (9). The hypercalcemic crisis is an unusual state of progressive and marked hyperparathyroidism producing kidney, intestine, central nervous system, cardiovascular system, and musculoskeletal system involvement with different symptoms such as polyuria, anorexia, vomiting, constipation, deterioration of mental status, confusion, weakness, dizziness, loss of appetite, and arrhythmia (10,11).Surgical intervention for parathyroidectomy is recommended for patients with symptomatic disease and complications like a hypercalcemic crisis (12).Acute pancreatitis is an inflammatory condition in which the pancreas is inflamed (1). The common causes of AP are biliary and gallstones, alcohol consumption, cigarette smoking, neoplasms, hypertriglyceridemia, medication toxicity, trauma from endoscopic retrograde cholangiopancreatography, abdominal trauma, various infections, autoimmune, ischemia, and hereditary causes (13). Pain, the most common symptom of AP, is often sudden and severe (more severe in the supine position), mainly in the upper abdomen (epigastric area), and may radiate to the back, chest, and flanks. In addition to pain, nausea and vomiting are common (13).
AP has different complications, including fluid accumulation around the pancreas, pseudocyst, intestinal involvement, infectious necrosis, vascular thrombosis, and renal failure, which may result in multi-organ failure and death (1,14,15). The pathophysiology of AP is exocrine and endocrine insufficiency of the pancreas due to the premature activation of proteolytic zymogens (16).
On the other hand, acute pancreatitis can be induced by hypercalcemia due to the secretory block, accumulation of secretory proteins, and possibly activation of proteases (17). According to the relationship between hypercalcemia with PTHP and hypercalcemia with AP, presenting PHPT with AP can be explained, and several studies reported this result based on their patients (5-7).
In the current work, we reported a case of hypercalcemia-induced acute pancreatitis caused by a functioning parathyroid adenoma, which recovered after medical therapy for PTHP and acute pancreatitis. This was followed by parathyroidectomy due to parathyroid adenoma to prevent the recurrence of hypercalcemia crisis and its related pancreatitis. During the postoperative follow-up, the patient presented no symptoms of hypercalcemia and abdominal pain, and the serum levels of PTH and calcium remained normal.
Therefore, we have shown that PHPT can be presented with symptoms of acute pancreatitis, and parathyroidectomy is an essential cure for parathyroid adenoma that results in complications of hypercalcemia prevention.
Conclusion
According to the current report, primary hyperparathyroidism may manifest as acute pancreatitis due to hypercalcemia. Therefore, we strongly recommend monitoring the serum calcium levels in patients diagnosed with acute pancreatitis. In the event of elevated levels, diagnostic and therapeutic interventions should be implemented for primary hyperparathyroidism to prevent the recurrence of pancreatitis and hypercalcemia.
Acknowledgements
The authors thank Dr Sima Aminoarroaya Lowe for providing helpful comments and for providing English language translation assistance during the preparation of this manuscript.
Funding
None.
Conflicts of Interest
Authors declare no conflict of interest.
Authors' Contribution
1-Maryam Karimi Fard: Patient physician and data collection and article writing.
2-Mohammadreza Shafiepour: Collaborator in writing the article.
3-Mahdieh Jamshidi: Collaborator in writing the article.
Received: 2023/02/22 | Accepted: 2023/07/7 | Published: 2023/10/29
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |