BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
URL: http://journal.zums.ac.ir/article-1-5703-en.html


 , Morteza Motedayen2
, Morteza Motedayen2 

 , Reza Hasanzadeh Makoui1
, Reza Hasanzadeh Makoui1 

 , Nima Motamed3
, Nima Motamed3 

 , Minoo Emami3
, Minoo Emami3 

 , Armin Bordbar1
, Armin Bordbar1 

 , Mohammad Reza Jamshidi4
, Mohammad Reza Jamshidi4 

 , Reza Madadi *5
, Reza Madadi *5 


2- Dept.of Cardiology, School of Medicine, Zanjan University of Medical Sciences, Zanjan, Iran
3- School of Medicine, Zanjan University of Medical Sciences, Zanjan, Iran
4- Dept. of Cardiac Anesthesiology, School of Medicine, Zanjan University of Medical Sciences, Zanjan, Iran
5- Dept. of Cardiology, School of Medicine, Zanjan University of Medical Sciences, Zanjan, Iran ,
✅ Our findings suggest that in STEMI patients, the chances of short-term complications such as post-MI mechanical complications, major arrhythmia, and bleeding requiring blood transfusion were lower in patients who were treated with primary PCI than those who received thrombolytic treatment. Also, the average hospitalization in CCU and hospital in the primary PCI group was lower than the thrombolytic group.
Acute myocardial infarction (AMI), the most prevalent manifestation of cardiovascular diseases, is primarily caused by coronary artery occlusion and associated with special clinical and paraclinical symptoms. AMI is presented in two forms, ST-elevation myocardial infarction (STEMI) and non-ST-elevation myocardial infarction (NSTEMI), which are accompanied by varying clinical outcomes. Due to the advanced coronary artery disease (CAD) and mechanical and/or electrical complications of AMI, patients (especially elders) with STEMI may experience a high mortality rate. STEMI is diagnosed based on clinical features and electrocardiographic evidence, as well as paraclinical findings (1). Generally, the typical chest pain, as well as electrocardiography (ECG) changes, ST-elevation of at least 1 mm in all leads except leads V2 and V3, represents definitive confirmation of STEMI. ST-elevation of at least 2 mm and 2.5 mm in leads V2 and V3 is considered STEMI in males aged more and less than 40 years, respectively. However, in females, the ST-elevation of 1.5 mm serves as a criterion for STEMI (1). Elevation in the serum levels of cardiac biomarkers, particularly troponin, along with cardiac clinical symptoms, can be used to determine AMI; however, cardiac markers may not be positive if the patient is timely referred to a treatment center (2).
In addition to pharmacologic therapies, including antiplatelet and antithrombotic agents, early and sustained reperfusion of the myocardium using the primary percutaneous coronary intervention (PCI) and through fibrinolysis is a vital part of a treatment strategy for AMI. The risk of death due to the myocardial infarction (MI) varies depending on the type of treatment, the onset of the symptoms, the risk of bleeding, the presence or absence of shock, and the patient’s transfer time to a primary PCI center. It is well demonstrated that time has a very crucial role in the establishment of reperfusion in STEMI, and 30-min delay in reperfusion causes an increase of 8% in the relative risk of death during the one year after MI. Therefore, rapid diagnosis and timely treatment can lessen the complications and improve the short-term and long-term outcomes of STEMI. However, patient's status, including age, sex, type of MI (anterior, inferior, etc.), blood pressure, and presence or absence of cardiac shock, as well as patient's Killip classification and the interval between the onset of symptoms and reperfusion following AMI may affect the treatment outcomes of the patients (3, 4).
Each reperfusion modality has its own complications, which are closely related to the physiological conditions of the patients. The most important and severe contraindication for fibrinolytic therapy is intracranial bleeding (5). While different kinds of therapies are available for patients with STEMI, reperfusion therapy is the most appropriate treatment for these patients (6). Previous studies have shown that STEMI patients treated with primary PCI has better clinical outcomes in the long term than those treated with thrombolysis. However, evidence has indicated no difference between these two therapeutic modalities within 2-3 hr after the MI (6, 7).
The aim of this study was to investigate the success rate of primary PCI and thrombolysis in reperfusion in STEMI patients and to study the short-term complications caused by these two methods.
During 2016-2017, we conducted this prospective cohort to investigate the short-term outcomes (30 days) of reperfusion by primary PCI or thrombolysis in patients with AMI referred to Ayatollah Mousavi and Valiasr Hospitals in Zanjan, Iran. Of these patients, only 180 cases with STEMI (MI with elevated ST segment) were selected for reperfusion therapies. Among the 180 patients included, 90 cases were chosen for primary PCI therapy and 90 cases for thrombolytic treatment. The <90 min door-to-balloon time guideline was taken into account to select STEMI AMI patients referring to the Ayatollah Mousavi Hospital for primary PCI therapy. In addition, patients who were diagnosed as STEMI at Valiasr Hospital were transferred to the Ayatollah Mousavi Hospital to undergo the primary PCI, considering the door-to-balloon time <120 min (the time elapsed between hospital admission and balloon inflation inside the infarct-related artery), otherwise the patients were stayed at the Valiasr Hospital for thrombolytic therapy.
The exclusion criteria included patients who did not agree to receive reperfusion or those who died before reperfusion, i.e. after 12 hours from the onset of MI pain. Patients who were candidates for thrombolytic therapy but had contraindications for this therapy were also excluded. These patients were transferred to a primary PCI center, if their door-to-balloon time was less than 120 minutes.
Clinical data and demographic characteristics of the patients, including the age, sex, weight, time of the pain onset, vital signs (e.g. heart rate and SBP [systolic blood pressure]), a detailed history of baseline diseases, other cardiovascular risk factors, were recorded at the beginning of the study. The type of MI (anterior, inferior, etc.) for each patient was verified based on the ECG results. After providing the initial emergency procedures and essential first-aid treatments, the patients were transferred to the catheterization laboratory, so-called cath lab, for coronary angiography before the primary PCI therapy. If the cath lab was busy (for any reason), or the patients had not consent for primary PCI, they underwent thrombolytic therapy. The success rate of coronary reperfusion by primary PCI and thrombolytic therapy was determined based on angiography and 90-min ECG, along with resolution or improvement of chest pain. Patients with ST recovery ≥50% in the 90-min ECG were considered to have successful reperfusion.
The definitive success of thrombolytic therapy was confirmed or rejected by subsequent angiography. The success of the two methods in angiography was determined based on thrombolysis in myocardial infarction (TIMI) flow grade. Moreover, non-invasive TIMI flow grading was used for reperfusion assessment. The studied patients were categorized into different groups considering their age, body weight, and SBP, as well as Killip classification. In this regard, patients were assigned into three subgroups of <65, 65-75, and >75, according to the age of STEMI onset. Regarding the bodyweight, the cases were subdivided into <65 kg, 65-89 kg, and >89 kg groups, and based on the level SBP, they were allocated into four subgroups of <100 mm-Hg, 100-140 mm-Hg, 141-160 mm-Hg, and >160 mm-Hg. The patients were also grouped into two categories of Class I and Class II-IV, according to their Killip classification. All the patients were examined for any signs of serious complications such as cerebrovascular accidents, shock, and heart failure 30 days after treatment. As mentioned above, the rate of reperfusion success for primary PCI and thrombolytic therapy was evaluated by angiography and compared based on the TIMI flow grade. Therefore, the patients were divided into four groups according to the TIMI flow criteria. The TIMI flow 0 was interpreted as no antegrade coronary flow beyond the occlusion, TIMI flow I was faint antegrade coronary flow beyond the occlusion with an incomplete filling of the distal coronary bed, TIMI-II was defined delayed or sluggish antegrade flow with complete filling of the distal coronary bed, and TIMI-III was described as normal coronary flow, which fills the distal coronary bed.
The 30-day treatment outcomes of the patients who received primary PCI or thrombolytic therapy were compared based on the following parameters: 1) death for any reason within 30 days, 2) cardiogenic shock, 3) congestive heart failure, 4) recurrent infarction, 5) death due to the cardiovascular diseases, 6) incidence of cerebrovascular accidents and stroke, 7) delayed reperfusion and MI type (inferior, anterior, etc.), 8) the rate of bleedings so that there is a need for blood transfusion, 9) the incidence of major arrhythmia (ventricular tachycardia and ventricular fibrillation), and 10) the rate of mechanical complications (free rupture of the ventricular wall and wall defect between ventricular).
This study was approved by the Ethics Committee of Zanjan University of Medical Sciences, Zanjan, Iran (ethical code: Zums.Rec.2015.274), and informed consent was obtained from all patients. Data were collected and analyzed by SPSS software version 20. P value <0.05 was considered a significant statistical level. Odds ratio (OR) was used to calculate for post-MI mechanical complications, major arrhythmia, bleeding complications (non-intracranial bleeding), TIMI flow grade III, and mortality in both treatment groups treated with primary PCI vs. the group treated with thrombolytic.
A total number of 180 AMI patients with ST-elevation hospitalized at Ayatollah Mousavi and Valiasr Hospitals were treated with primary PCI and thrombolysis.
The demographic characteristics of patients in each group are shown in Table 1. The two groups (primary PCI group and thrombolytic group) were not significantly different in terms of confounding factors such as sex, age, high blood pressure, underlying disease, and history of smoking; therefore, they were compared.
Table 1. Demographic information and basic characteristics of patients in each of the studied groups
| Primary PCI group | Thrombolytic therapy group | ||||
| Frequency (%) | Percentage (%) | Frequency (%) | Percentage (%) | ||
| Sex | Male | 68 | 75.6 | 69 | 76.7 |
| Female | 22 | 24.4 | 21 | 23.3 | |
| Age Group (Year) |
>65 | 52 | 57.8 | 54 | 60 |
| 65-75 | 24 | 26.7 | 27 | 30 | |
| 75≥ | 14 | 15.6 | 9 | 10 | |
| Weight (kg) |
65 < | 6 | 6.7 | 2 | 2.2 |
| 65-75 | 76 | 84.4 | 85 | 94.4 | |
| 75≥ | 8 | 8.9 | 3 | 3.3 | |
| Having at least one underlying positive illness | 58 | 64.4 | 66 | 73.3 | |
| Smoke user: positive | 28 | 31.1 | 42 | 46.7 | |
| BP systolic (mmHg) |
>100 | 12 | 13.3 | 5 | 5.6 |
| 100-140 | 49 | 54.4 | 54 | 60 | |
| 141-160 | 12 | 13.3 | 16 | 17.8 | |
| 160< | 17 | 18.9 | 15 | 16.7 | |
| Troponin results | + | 78 | 86.7 | 86 | 95.6 |
| _ | 18 | 13.3 | 4 | 4.4 | |
| Infarctus site | Anterior | 57 | 63.3 | 49 | 54.4 |
| Inferior | 33 | 36.7 | 41 | 45.5 | |
BP: Blood pressure
In the primary PCI group, 68 (75.6%) out of 90 patients were males, and the remaining 22 (24.4%) cases were females. However, in the thrombolytic group, 69 (76.6%) out of the 90 patients were males, and 21 (23.3%) cases were females. The mean age of males and females in first and the second groups were recorded as 59.19 ± 12.72 and 67.82 ± 10.30, respectively. The mean age of males and females in both patient groups was 60.67 ± 11.33 and 63.67 ± 10.11, respectively.
Our findings showed that 64.4% of patients in the first group and 73.3% in the second group had a history of DM, HTN, HLP, MI, PCI, or CABG, indicating the high frequency of these complications among patients who received thrombolytic therapy (Figure 1). HTN and HLP were found as the main comorbidities in the primary PCI (first) group, whereas DM was the underlying disease with the highest frequency in the thrombolytic (second) group.
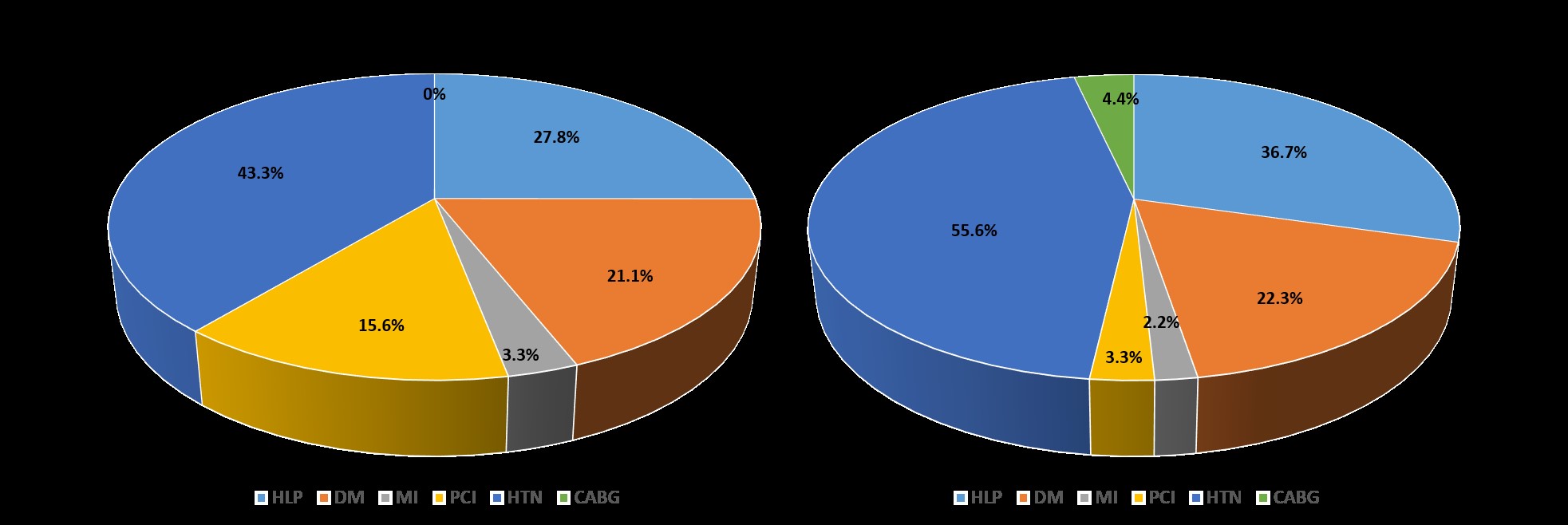
Figure 1. Frequency of each underlying disease in primary PCI group (left) and thrombolytic treatment group (right).HLP: hyperlipidemia; DM: diabetes mellitus; MI: myocardial infarction; PCI: percutaneous coronary intervention; HTN: Hypertension; CABG: coronary artery bypass grafting
The SBP of 100-140 mmHg was the highest pressure among 54.4% and 60% of patients in the first and the second groups, respectively. According to the results, a statistically significant difference was found between SBP with age (p <0.009) and weight (p <0.03). The troponin levels were observed to be positive in 86.7% of patients in the primary PCI group and 95.6% in the thrombolytic group. Also, 63.3% and 36.7% of first patient group and 54.4% and 45.5% of the second patient group had anterior and inferior infarction, respectively, suggesting that most of the patients in both groups have experienced anterior infractions. For patients of the primary PCI group with anterior infarction, the SBG of 100-140 mmHg and SBP less than 100 mmHg were found to be the highest and lowest levels of blood pressure, whereas for patients with inferior infarction, 100-140 mmHg and 141-160 mmHg were observed as the highest and lowest blood pressure level, respectively. The SBG of patients in the thrombolytic therapy group with anterior and anterior infarction were 100-140 mmHg and less than 100 mmHg, as the highest and lowest blood pressure, respectively.
The mean ± SD of the door-to-balloon time/door-to-needle time for the patients receiving primary PCI and thrombolytic therapy was 63.95 ± 23.92 min and 53.70 ± 21.52 min, respectively. Moreover, in almost all patients in both groups, the door-to-balloon time/door-to-needle time was not exceeded 120 min. The minimum and maximum door-to-balloon time for the primary PCI group was recorded as 12 min and 114 min, while that of door-to-needle time for the thrombolytic therapy was 10 min and 115 min, respectively. The results indicated no statistically significant difference between the two measurement indices and demographic characteristics of the patients, including age, weight, SBP, the length of CCU admission, and the duration of hospitalization. The average length of stay in the CCU and the overall hospital stay for the primary PCI group was 56.57 ± 0.55 hrs and 122.29 ± 82.27 hrs, but for patients of thrombolytic group, they were 96.74 ± 29.32 hrs and 154.72 ± 39 hrs, respectively. The difference between the duration of hospitalization and the patient’s age was statistically significant (p <0.04).
The information related to TIMI flow grade, Killip classification, angiography reports, mechanical complications of MI, major arrhythmia, and mortality in 30 days in the studied patients is given in Table 2. Post-MI mechanical complications, such as mitral regurgitation/stenosis, ventricular septal defects, or ventricular septal rupture, were detected only in 1.1% and 4.4% of patients who underwent primary PCI and thrombolytic therapy, respectively.
Table 2. Frequency and percentage of variables in patient groups
| Primary PCI | Thrombolytic therapy | ||||
| Frequency (N) | Percentage (%) | Frequency (N) | Percentage (%) | ||
| TIMI flow grade | 0 | 5 | 5.6 | 11 | 12.2 |
| I | 1 | 1.1 | 15 | 16.7 | |
| II | 8 | 8.9 | 39 | 43.3 | |
| III | 76 | 84.4 | 25 | 27.8 | |
| Killip classification | I | 65 | 72.2 | 52 | 57.8 |
| II-IV | 25 | 27.8 | 38 | 42.2 | |
| Angiography report |
SVD | 26 | 28.9 | 21 | 23.3 |
| 2VD | 33 | 36.7 | 36 | 40 | |
| 3VD | 31 | 34.4 | 33 | 36.7 | |
| Mechanical complication MI | MR | 0 | 0 | 3 | 3.3 |
| VSD | 0 | 0 | 1 | 1.1 | |
| Rupture of the ventricle wall | 1 | 1.1 | 0 | 0 | |
| None | 89 | 98.9 | 86 | 95.6 | |
| Major arrhythmia | VF | 5 | 5.6 | 6 | 6.7 |
| VT | 7 | 7.8 | 11 | 12.2 | |
| None | 78 | 86.7 | 73 | 81.1 | |
| Mortality within 30 days | 8 | 8.9 | 4 | 4.4 | |
TIMI: thrombolysis in myocardial infarction; MI: myocardial infarction; SVD: single vessel coronary artery disease; 2VD: two vessels coronary artery disease; 3VD: three vessels coronary artery disease; VF: ventricular tachycardia; VT: ventricular fibrillation
No patient with intracranial hemorrhage (ICH) was identified in the primary PCI group, but one (1.1%) case with ICH was detected in the thrombolytic therapy group. Our findings revealed that bleeding complications (other than intracranial hemorrhage) following reperfusion with primary PCI was detected in only one case (1.1%) who needed a blood transfusion; however, patients who received thrombolytic therapy were more prone to bleeding complications, and 8 (8.9%) cases had bleeding and needed a blood transfusion. Furthermore, we observed a higher mortality rate among patients (8 out of 90 cases; 8.9%) treated with primary PCI than those (4 out of 90 cases; 4.4%) who received thrombolytic therapy.The OR for short-term complications and TIMI flow grade of primary PCI vs. thrombolytic therapy in STEMI patients are given in Table 3. The OR of mechanical complication MI, major arrhythmia, and bleeding complications requiring blood transfusion (except ICH) in patients of primary PCI group was 0.24, 0.66, and 0.11 respectively. Also, OR for TIMI III and that of death among the patients of the first treatment group were 14.45 and 2.12, respectively.
Table 3. Odds ratio for short-term complications and TIMI flow grade of primary PCI versus thrombolytic therapy
|
Odds ratio |
|
Variable |
|
0.24 |
|
Mechanical complication MI |
|
0.66 |
|
Major arrhythmia |
|
0.11 |
|
Bleeding complications needed blood transfusion (except ICH) |
|
2.12 |
|
Mortality within 30 days |
|
0.42 |
0 |
|
|
0.05 |
I |
TIMI flow grade |
|
0.12 |
II |
|
|
14.45 |
III |
|
MI: myocardial infarction, ICH: intracranial hemorrhage; TIMI: thrombolysis in myocardial infarction
Discussion
Cardiovascular disease (CVD) is the leading cause of mortality worldwide. High blood pressure, dyslipidemia, metabolic syndromes, and inappropriate lifestyles are known as the main risk factors predisposing to CVD (8). Based on the reports, the prevalence of CAD and associated mortality rates have increased in recent years. MI is the most common form of CAD, leading to heart failure (9, 10). AMI with ST-elevation results from sudden and complete obstruction of a major coronary artery by a blood clot (11).
Recently, a breakthrough is made in the treatment of AMI through the application of new treatment strategies. Nowadays, reperfusion with the primary PCI is a standard treatment for patients with STEMI (12, 13). In this study, 90 patients were enrolled in the primary PCI treatment group, of these 90 cases, 75.6% and 24.4% were females and males, respectively. Moreover, 76.6% and 23.3% of patients in the thrombolytic therapy group were males and females, respectively. The number of patients with anterior infarction was found to be about 30% higher than those with inferior infarction in the primary PCI group. However, in thrombolytic group, the number of patients with anterior and those with inferior MI localization was the same. Moreover, in both treatment groups, patients were frequently of TIMI-III and TIMI-II, while the least of patients were of TIMI-0. Similar to our findings, Ge et al. (2013) demonstrated that after therapeutic interventions, 82% of patients who underwent thrombolysis had TIMI-III flow, whereas 88% of treated cases in the primary PCI group had TIMI-III flow (14). According to our results, no ICH was observed in the primary PCI group, while one (1.1%) patient had ICH among those who received thrombolytic therapy. Moreover, bleeding complications (other than intracranial hemorrhage) were less common following reperfusion with primary PCI, and only one case (1.1%) experienced bleeding and needed a blood transfusion. However, patients who received thrombolytic therapy were more prone to bleeding complications, and 8 (8.9%) patients had bleeding requiring a blood transfusion. Armstrong et al. (2013) conducted a study to investigate the efficacy of prehospital thrombolysis and primary PCI in 1,892 patients who were unable to undergo primary PCI within 1 hour. They explored that the primary endpoint (a composite of death, shock, congestive heart failure, or reinfarction up to 30 days) occurred in 14.3% of the primary PCI group and 12.4% of the thrombolytic group. Moreover, their results revealed that more intracranial hemorrhages (p = 0.04) occurred in the fibrinolysis (1%) group than in the primary PCI group (0.2%); however, the rates of non-intracranial bleeding were similar in the two groups (15). In our study, the average door-to-balloon time for patients who received primary PCI was 63.95 ± 23.92 min and the mean door-to-needle time for the thrombolytic therapy group was 53.70 ± 21.52 min. In the study of Ge et al. (2013), the time elapsed between the onset of symptoms and reperfusion was the same for both groups, though a significant difference with p <0.001 was observed between the door-to-needle time (45 ± 23 min) and the door-to-balloon time (88 ±44 min) (14). In another study conducted by Widimsky et al. (2002), the door-to-balloon time for the primary PCI group and door-to-needle time for the thrombolytic treatment group were 97 ± 27 min and 12 ± 10 min, respectively. They found a significant correlation (p ≤0.05) between the door-to-balloon time/door-to-needle time with the 30-day mortality rate, which was 10.4% in the PPCI group and 6% in the thrombolytic group. The mortality rate in the thrombolytic therapy group was 15.3% and in the PPCI group was 8.4% (16). According to our findings, the average length of stay in the CCU and the overall hospital stay for the thrombolytic group was greater than that of the primary PCI group. Moreover, in the study of Henriques et al. (2005), a mortality rate of 31% was found in patients with thrombolytic therapy, while this rate was reported as 22% in cases who received the primary PCI. Moreover, the non-lethal MI was about 7% in the primary PCI group and 22% in the thrombolytic group (17). In our study, 98.9% of patients in the primary PCI group and 95.6% of the patients in thrombolysis group did not experience post-MI mechanical complications; hence, post-MI mechanical complications were less frequent in the first patient group than the second group (OR = 0.24). Besides, we observed a higher mortality rate in patients treated with primary PCI (8.9%) than those who received thrombolytic therapy (4.4%), with OR = 2.12. Different mortality rates among those who received primary PCI and thrombolysis have also been reported by several studies. In this regard, Claeys et al. (2011) have reported a 5.9% mortality rate for the patients treated with primary PCI vs. 6.6% in the thrombolytic therapy group (18). In addition, the mortality rate for high-risk individuals was reported to be 0.3% by the primary PCI treatment and 0.4% by the thrombolysis. Busk et al. (2007) have investigated the benefit of inter-hospital transfer for primary angioplasty compared to on-site fibrinolysis at 30-day follow-up. They found that the composite endpoints (death, clinical reinfarction, or disabling stroke) significantly (p = 0.006) reduced in the primary PCI when compared to fibrinolysis at three years (19.6% vs. 25.2%). Their results also showed that in patients transferred to primary PCI compared to those receiving on-site fibrinolysis, the composite endpoint reduced significantly (p = 0.007) and occurred in 20.1% vs. 26.7%, i.e. death in 13.6% vs. 16.4% (p = 0.18), clinical reinfarction in 8.9% vs. 12.3% (p = 0.05), and disabling stroke in 3.2% vs. 4.7% (p = 0.23) (19). Dieker et al. (2004) have reported that the 70-95% of STEMI patients who transferred to the primary PCI instead of on-site thrombolysis had TIMI-III flow, while only 50-70% of patients who were treated with the thrombolytic therapy had TIMI-III flow. They also showed that the mortality rate significantly (p = 0.02) reduced in patients who transferred to primary PCI compared to on-site thrombolytic therapy (4.4% vs. 6.55%).
A mortality rate of 9.6% was observed in patients who underwent thrombolytic therapy; however, in patients receiving the primary PCI, the mortality rate was 6.8% (20). In contrast to our study, Steg et al. (21) have shown that the 30-day mortality rate in patients who were randomized less than 2 hours after the symptom onset and treated with primary PCI was 5.7%, while the mortality rate of 2.2% with a significant difference (p = 0.058) was observed in patients treated with thrombolysis during the 30 days of follow up. Moreover, the cardiogenic shock was found to be 5.3% and 1.3% in the primary PCI and thrombolytic groups, respectively, with a significant difference of p = 0.032. Interestingly, they displayed that unlike the primary PCI group (5.9%), the randomized patients (3.7%) in the thrombolytic group experienced a higher mortality rate ≥2 hours after the symptom onset, with a significant difference of p = 0.47 (21). We speculate in the present study that the inter-hospital transfer of patients to the primary PCI who were predisposed to the cardiogenic shock may be responsible for the higher mortality rate in the primary PCI group. One of the most limitations of this study was the absence of thrombolytic therapy with less side effects. Also, the lack of 24-hour, seven-day coverage of primary PCI and the presence of only one active cath lab in Mousavi Hospital caused the shift of some STEMI patients to Valiasr hospital for thrombolytic therapy.
Conclusion
Overall, the present study suggested that primary PCI leads to a higher reperfusion rate (TIMI-III in 84.4%) in STEMI patients. In this study, no significant difference was found between door-to-balloon time/door-to-needle time and the age, weight, and SBP of patients, as well as the duration of hospitalization in CCU and hospital. However, there was a significant difference between total hospital stay and age (p <0.04). Moreover, the rate of complications after myocardial infarction, such as mechanical complications and major arrhythmias, was lower in patients of the primary PCI group than in the patients of the thrombolytic group.
Acknowledgements
None.
Conflicts of Interest
None.
Received: 2021/04/4 | Accepted: 2022/03/3 | Published: 2022/12/12
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |



