BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
URL: http://journal.zums.ac.ir/article-1-6138-en.html


 , Fereshteh Majlessi2
, Fereshteh Majlessi2 

 , Yadollah Jannati3
, Yadollah Jannati3 

 , Sayed Abolhasan Naghibi4
, Sayed Abolhasan Naghibi4 

 , Ali Ghaemian5
, Ali Ghaemian5 

 , Alireza Sangani6
, Alireza Sangani6 


2- Dept. of Health Education and Promotion, School of Public Health, Tehran University of Medical Sciences, Tehran, Iran.
3- Dept. of Nursing, Faculty of Nursing, Mazandaran University of Medical Sciences, Sari, Iran.
4- Health Sciences Research Center, Mazandaran University of Medical Sciences, Sari, Iran.
5- Dept. of Cardiology, Faculty of Medicine, Cardiovascular Research Center, Mazandaran University of Medical Sciences, Sari, Iran.
6- Dept. of Psychology, Ahvaz Branch, Islamic Azad University, Ahvaz, Iran.
✅Providing opportunities for further social support for MI patients paves the way for enhancing health-promoting behaviors and reducing depression in this group of patients.
Depression, as a prevalent mental health disorder worldwide, plays a critical role in enhancing the global burden of diseases (1). Major depressive disorder (MDD) is a mood disorder characterized by a persistent feeling of low mood, loss of pleasure and interest, weight loss, insomnia, fatigue, emptiness, psychomotor slowness, guilt, diminished concentration, and the recurrent thoughts of death (2).
Among mental disorders, MDD accounts for the largest portion (40.5%) of disability-adjusted life years (DALYs) (3). In Asia, the prevalence of depression is estimated to be about 7.8%-34.8% in adults (4). In general, more than 300 million individuals of different ages suffer from this disorder (5). According to the reports, one-fifth of Iranians are affected by depression. A national study on the burden of diseases and injuries indicated that mental illnesses and behavioral disorders are the second leading cause of health problems in Iran. In addition to intentional and unintentional incidents, depression is the third most prevalent health problem in the country.
Considering the relatively high prevalence of depression and the significant burden of this disease for patients, health systems, and societies, further studies are recommended for adopting appropriate treatment approaches, prevention measures, and management practices (6). Although the risk factors of depression are well detected, the preventive factors have less been researched (3). Social support is introduced as one of these effective factors. The concept of social protection means protecting people from mental health problems and works through the benefits of social relationships as a protective shield against stressful situations (1). In addition to physical problems, cardiovascular patients face psychological problems, such as anxiety and depression. As a result, understanding the relationship between disease perception and disease outcomes can affect the quality of life in patients (7).
Depression is one of the major medical and social problems, which is considered the most common comorbid disorder in many medical conditions, especially heart disease (8). Some studies have revealed a significant relationship between depression and perceived social support in patients with heart disorders (9-12). Bucholz et al. showed that the low levels of social support in myocardial infarction (MI) patients were associated with a poor health condition and higher levels of depression (13). Leifheit-Limson et al. also concluded that cases with less social support had a lower mental function and revealed more depressive symptoms during 12 months, in comparison to the patients receiving higher support (14).
However, the exact relationship between social support and depression is still unknown (15). In a clinical trial, a negative relationship was found between depression and social support, which may be due to the social support of friends rather than family. It is a fact that social support by friends is more understood among younger individuals (16). This finding suggests that the specific domain of social support plays a vital role in improving or diminishing depression (15).
Moreover, previous studies have indicated that negative statements and the lack of social qualification exhibited by depressed patients may disrupt their social relationships (17, 18). Moreover, it is proved that depressed and susceptible people develop negative responses and have problems in interactions with others making others stay away from them (16). The results of an epidemiological study indicated that a healthy lifestyle, such as having a proper diet, not smoking, maintaining an ideal weight, and physical activity can be effective in controlling cardiovascular risk factors (19).
This survey was designed due to the lack of a precise relationship between social support and depression (15-18) and the value and social importance of (15-18) and the value and social support importance. . The cited resource may be very helpful for cardiovascular patients to tackle their psychological and physical problems. Therefore, the present study aimed to assess the role of perceived social support in predicting MDD and lifestyle components in MI patients.
This quasi-experimental study was conducted on MI patients of Mazandaran Heart Center Hospital, Iran in 2019. This study was approved by the Ethics Committee of Mazandaran University of Medical Sciences with the code of NO.IR.MAZUMS.REC.13971105. To follow the research ethics, a letter of introduction was obtained from the research deputy of Mazandaran University of Medical Sciences and was submitted to the head of Mazandaran Heart Center Hospital.
Following being introduced to the study participants, the research objectives were explained to them. The subjects were informed that participation in the study was voluntary and the consent forms were signed. To ensure the confidentiality of the collected data, the names of patients were not written on the information sheets.
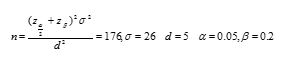
In this study, purposive and convenience sampling methods were adopted. The sample size was considered as 176 patients based on the sample size formula. The inclusion criteria were willingness to participate in this study, the lack of emergency conditions, full consciousness at research time, no previous history of depression according to the recorded documents and the history of the patient, and at least five days being passed from cardiac infarction. The exclusion criteria entailed unwillingness to participate in this study and serious emergency conditions. The sample size was estimated based on the results of the study carried out by Leifheit-Limson (14) and the following equation:
Three standard questionnaires were utilized to collect the required data.
1.Social Support Appraisals (SS-A) Scale by Phillips
2.Beck Depression Inventory (BDI-II)
3.Health-Promoting Lifestyle Profile (HPLP-II)
Statistics Analysis
The data were collected from the files and direct interviews of patients and were analyzed using the SPSS software version 23 (IBM, Ill., USA). Descriptive statistics, including the mean and standard deviation were used to describe the data for quantitative variables, such as social support components and qualitative variables, such as gender. Pearson correlation coefficient and canonical correlation coefficient were employed to analyze the data and evaluate the relationships between the variables. The significance level was considered as P-value<0.05.
The mean age of the participants was 12.5±54.59 years. The majority (89.2%) of the participants were married, 23.3% were retired, and 37.5% had elementary education. The mean time interval between MI and interview was 7.5±0.75 days. All questionnaires were filled out by patients at the time of hospitalization.
Table 1. Frequency of demographic variables in MI patients
| N (%) | Variable | |
| 178(72.9) | Male | Gender |
| 48(27.3) | Female | |
| 8(4.6) | Single | Marital status |
| 11(6.3) | widow | |
| 157(89.2) | Married | |
| 66(37.5) | Elementary | Level of education |
| 42(23.9) | Diploma | |
| 15(8.5) | Associate Degree | |
| 19(10.8) | MA/BS | |
| 18(10.2) | MA/MS | |
| 16(9.1) | Others | |
| 25(14.2) | Clerk | Occupation |
| 29(16.3) | Farmer | |
| 35(19.9) | Self-employed | |
| 41(23.3) | Retired | |
| 38(21.6) | housewife | |
| 8(4.5) | Others | |
Table 2. Mean and standard deviation of lifestyle components, social support and depression in MI patients
| Mean | SD± | Variable |
| ±12.50 | 54.29 | Age |
| 0.31± | 18.32 | Social support |
| ±0.79 | 13.60 | Depression |
| ±7.01 | 146.47 | lifestyle |
According to Table 2, the depression level was low (13.6±0.79) among patients with good social support (18.32 ±0.31). Moreover, the lifestyle of patients was moderate (146.47±7.01).
As could be observed in Table 3, social support affected lifestyle components significantly. Our findings demonstrated that social support predicted and significantly influenced health accountability (R2=0.691, β=0.289), spiritual growth (R2=0.672, β=0.256), stress management (R2=0.285, β=0.122), and interpersonal behavior (R2=0.586, β=0.175).
Table 3. Canonical correlation coefficients in predicting lifestyle components (benchmark variable) regarding to social support (predictive variables)
| Independent variable | Canonical functions | Canonical correlation | R2 | Effect (B) | t | p |
| Social support | Health accountability | 0.355 | 0.691 | 0.289 | 4.108 | 0.001 |
| Physical activity | 0.336 | 0.113 | 0.048 | 1.112 | 0.527 | |
| Nutrition | 0.831 | 0.126 | 0.016 | 0.236 | 0.639 | |
| Spiritual growth | 0.534 | 0.672 | 0.256 | 4.844 | 0.001 | |
| Stress management | 0.819 | 0.285 | 0.122 | 2.124 | 0.001 | |
| Interpersonal behavior | 0.765 | 0.586 | 0.175 | 4.968 | 0.001 |
Table 4. Mean, standard deviation, and Pearson correlation coefficient matrix for the relationship between social support and depression
| variable | M | SD | Perceived stress | Physical symptoms |
| Social support | 16.71 | 2.82 | 1 | |
| Depression | 14.25 | 11.60 | -0.47** | 1 |
**p≤0.01
The results summarized in Table 4 indicated an indirect correlation between social support and depression (r=-0.47, P<0.01). As shown in Table 5, regarding the value of R2, social support could predict depression by 0.479. Furthermore, the value of β indicated that social support imposed a negative effect on depression (-0.479).
Table 5. Multiple correlation coefficient, beta coefficients, determination coefficient, and standard error
| Predictive variables | R | R2 | Adjusted R-squared | SE | Coefficient F | Sig. | Coefficient of effect |
| Social support | 0.479 | 0.229 | 0.214 | 10.292 | 52.326 | 0.001 | -0.479 |
Discussion
This study aimed to examine the role of perceived social support in predicting MDD and lifestyle components in MI patients. Our results indicated a statistically significant reverse correlation between the level of social support and depression. The latter finding has been supported by many other studies (27-29).
In a study by Su et al., the correlation between social support and depression was reported to be -0.48 (30) and the value obtained in the present study was -0.47. Leifheit-Limson et al. concluded that patients with lower social support had lower quality of life and experienced more depressive symptoms (14). The study conducted by Liu showed that social support may act as a flexibility factor against long-term cardiovascular risk, which is related to depression (31). Compare et al. investigated the roles of social support and depression in cardiovascular patients. These authors reported that depressive symptoms and the lack of social and family supports were associated with disease progression (11).
On the other hand, social support in the present study could predict depression by 47%. Consistent with our findings, the prediction powers were 43.7% and 42% in the studies carried out by Su (30) and Miller (21), respectively. These findings would help clinical staff to understand the physical and mental problems of cardiovascular patients. Accordingly, we suggest that the early prediction of depression and adequate social support may improve the conditions of patients in the face of disease and promote the quality of health care services.
To sum up, social support is an available potential resource, which can be strengthened and bring benefits to individuals. In this regard, the critical role of the family should be taken into consideration. Family can act as an information source with instrumental and emotional supports that reduce the depression symptoms in patients. Therefore, we recommend further investigations and researches about social support and its components.
According to the findings of this study, social support had a significant effect on lifestyle components. It predicted lifestyle components, including health accountability, spiritual growth, stress management, and interpersonal behavior by 69%, 67%, 28%, and 58%, respectively. Roming et al. concluded that low stress, high spirituality, and social support correlated significantly with high and medium levels of quality of life in patients. In other words, spiritual growth and social support are the basic adaptation factors in terms of a better quality of life (22). Furthermore, various studies have indicated a positive and significant correlation between social support and lifestyle (23, 32). A study in Thailand on women with cervical cancer showed that social support was effective in lifestyle as one unit increase in social support promoted lifestyle behaviors by 0.7 unit (33).
In contrast, Brooks et al. reported that health-promoting lifestyle factors did not significantly correlate with perceived social support factors (34). The investigation performed by Brooks aimed to evaluate the relationship of social support and lifestyle habits with weight loss during 18-24 months after obesity surgery. The non-significant relationship between social support and lifestyle might be due to more attention to diet and other lifestyle principles in the first days after treatment. In addition, families provide more support to the patients during the first days, which may cause such a result. However, the lifestyle and family support of patients are gradually disregarded over time. Consequently, it is necessary to highlight the significance of this issue for patients and their families.
Conclusion
Undoubtedly, lifestyle modification in its general sense, psychologically and physically, can be one of the best ways to prevent the occurrence of various diseases in humans. Fortunately, today, improved public awareness has increasingly caused people to check the health of their lifestyle. Moreover, related clinics and counseling centers are expanding in developed countries.
It should be noted that an augmentation in social supports may lead to reduced depressive symptoms and elevated health-promoting behaviors in patients. It is needed to provide opportunities for further social supports of patients through services and interventions, which improve social skills. Furthermore, healthy lifestyle patterns can be taught to others by holding workshops and effective training courses.
Limitations
Study limitations included self-report by patients, which may tempt them to present a better picture of their social support, depression, and lifestyle.
Acknowledgements
we acknowledge the patients who participated in the research. The authors are grateful to the Vice Chancellor for research, Mazandaran University of Medical Science.
Conflicts of Interest
The authors declare no conflicts of interest
Received: 2020/07/24 | Accepted: 2021/02/22 | Published: 2021/02/28
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |