BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
URL: http://journal.zums.ac.ir/article-1-6625-en.html


 , Seyed Mohammad Hassan Moallem1
, Seyed Mohammad Hassan Moallem1 

 , Monavar Afzalaghaee2
, Monavar Afzalaghaee2 

 , Farzad Omidi-Kashani *3
, Farzad Omidi-Kashani *3 


2- Dept. of Biostatistics and Epidemiology, Faculty of Medicine, Mashhad University of Medical Sciences, Mashhad, Iran
3- Dept. of Orthopedic Surgery, Faculty of Medicine, Mashhad University of Medical Sciences, Mashhad, Iran ,
✅ Although all types of refractory L4-L5 LDS benefit from the operation, this improvement is not different among the types. It seems here, like other areas of the spine, that no significant relationship exists between the clinical and radiological characteristics.
Lumbar Degenerative spondylolisthesis (LDS) is a common spinal disease in middle age and older adults with a prevalence of 4% in the general population (1). Most of the cases with LDS are asymptomatic and fortunately, and most of the symptomatic patients respond favorably to routine conservative treatment including drugs, physiotherapy, and lifestyle modification (2). In few cases, clinical complaints remain refractory or neurologic deficit appears and these peculiar cases finally need surgery (3, 4).
Meyerding classification is an old, popular, and still, practical classification proposed to categorize lumbar spondylolisthesis based on the severity of vertebral slippage (5). This classification has 5 types; every 25% of vertebral slippage over the adjacent below vertebra gets one type and in type 5, vertebral spondyloptosis occurs. The major disadvantage of this classification in LDS is its inability to classify the disease into different groups and most cases are placed in type 1 or rarely 2. Another limitation is that other radiologic parameters (such as kyphosis and disc height) as well as clinical characteristics are not considered (6). In 2015, a new classification called Clinical and Radiographic Degenerative Spondylolisthesis (CARD classification) was introduced to address these limitations (7). If different types of LDS in CARD classification could show different clinical features and responses to treatment, then CARD classification can be more effective and helpful in clinical practice. This study aims to investigate the clinical significance of CARD classification based on clinical outcomes of the disease using valid questionnaires and assessment methods.
First of all, we recorded our proposal in the Deputy of Research, Mashhad University of Medical Sciences with a record number of 980443. Ethical considerations were observed following the instructions of the ethics committee of Mashhad University of Medical Sciences (approval number: IR.MUMS.MEDICAL.REC.1398. 504). In this retrospective study, we assessed all the patients who underwent decompression, fusion and instrumentation surgery due to LDS from February 2015 to January 2019 in Imam Reza Hospital, Mashhad. Inclusion criteria were: 1) mono-segment degenerative spondylolisthesis in L4-L5 level, 2) similar surgical technique (decompression, an attempt to reduce the slipped vertebra, fusion and instrumentation with pedicle screw and rod). Transforaminal lumbar interbody fusion was carried out only in those cases with local kyphosis correction, the small surface area of the transverse processes (<2cm2) or major slippage reduction (>25%) to promote stabilization, fusion, and rehabilitation. As in LDS, the severity of slippage is usually low, and we only fused the slipped vertebra to the stable one below. We excluded the patients with LDS other than L4-L5 level, patients with other types of spondylolisthesis, multi-level LDS, revision surgeries, patients with significant co-morbidity (end-stage renal disease, uncontrolled diabetes, immunodeficient patients, etc.), and those with a follow-up period of fewer than two years. Informed consent was obtained from all the patients and no coercion was used to fill out the information form. Participants were assured that their information would remain confidential and would never be disclosed individually. Surgical technique was the same throughout this period and all surgeries were carried out by the surgical team of the senior author (F.O.K).
According to CARDS classification, we placed our patients into four radiographic types (7):
Type A: Characterized by intervertebral disc space collapse (bony apposition) but no significant kyphosis. Disk space collapse may be symmetrical or asymmetrical.
Type B: Relative preservation of disc space with anterior vertebral slippage £ 5mm in all lateral views.
Type C: Relative preservation of disc space with anterior vertebral slippage > 5mm on at least one of the lateral radiographs.
Type D: The presence of segmental kyphosis in at least one of the lateral views.
Clinical assessment based on CARDS has only one item; leg pain modifier: no pain (score 0), unilateral (score 1), and bilateral (score 2). As the design of our study was retrospective, this modifier could not be precisely obtained. On the other hand, the sample size was relatively small and too many sub-categories would consequently diminish the value of the results. Therefore, we did not evaluate this variable.
All the patients had Flexion-extension standing radiographs and lumbosacral MRI at the time of admission. All of these patients filled out the standard questionnaires including the Oswestry Disability Index (ODI) and Visual Analogue Scale (VAS) at preoperative and final follow-up visits (8, 9). Oswestry disability index is the most common method of assessing patients with lumbar disorders, which has also been translated into Persian and its reliability and validity have been proven (10). The questionnaire consisted of 10 questions, each scored from 0 (minimum disability) to 5 (maximum disability) and finally expressed as a percentage of disability. A recovery greater than 10 (20%) was assessed as a clinically significant improvement. Pain assessment in the leg and the lumbar area was carried out with Visual Analogue Scale (VAS) which varies from zero to ten (9).
Finally, the relationship between different types of LDS and the patient's clinical symptoms was statistically analyzed to determine whether there was a relationship with the severity of symptoms or patients' response to surgical treatment.
All statistical analyzes were performed using the SPSS software (SPSS Inc, Chicago, Illinois, USA, version 22.0). Data are presented as mean± standard deviations and ratios appropriately. Nonparametric and parametric variables without normal distribution were compared using the Kruskal-Wallis test. Parametric variables were compared using the t-test.
At the beginning of the study, 60 patients met the study criteria, but during the study, nine patients could not be followed-up and two died during this period. Finally, 49 patients were fully evaluated, 11 patients (22.4%) male and 38 female (77.6%). The mean age of the patients was 56.8 ± 9.8 (range: 33 to 76 years old). Body mass index (BMI) was normal only in 26.2% of the patients. The mean follow-up period was 40.5±6.8 months (range: 26 -72 months). Demographic characteristics are summarized in Table 1.
Table 1. Demographic variables in the study
| Count | N (%) | ||
| Sex | M | 11 | 22.4 |
| F | 38 | 77.6 | |
| Age | < 50 years old | 13 | 28.9 |
| 50 - 60 years old | 16 | 35.6 | |
| > 60 years old | 16 | 35.6 | |
| BMI | Normal | 11 | 26.2 |
| Overweight | 19 | 45.2 | |
| Obese | 12 | 28.6 | |
Table 2 shows the age and BMI in different types; the age distribution between the types was not statistically significant, although the oldest patients were more commonly placed in type A. Table 2 shows the severity of pain (in both leg and back) and disability in preoperative, postoperative, and the amount of improvement with surgery. Although based on the paired t-test, surgery in all types of LDS could dramatically improve both pain and disability, no significant difference was observed between the types.
The mean BMI had a significant difference across types; patients in type C had a significantly higher BMI than those in types D and A. Gender distribution was similar across the four types (Figure 1).
Table 2. variables in each type
| Type A | Type B | Type C | Type D | P value | ||
| Number | 7(14.6%) | 21(43.8%) | 10(20.8%) | 11(22.4%) | 0.128 | |
| Age | 61.5±9.9 | 55.7±10.4 | 56.4±10.5 | 56.6±8.4 | 0.662 | |
| BMI | 24.8±2.1 | 27.7±3.9 | 29.8±2.3 | 25.4±3.2 | 0.012* | |
| Sex | Male | 4(57.1%) | 4(19.0%) | 1(10.0%) | 2(20.0%) | 0.171 |
| Female | 3(42.9%) | 17(81.0%) | 9(90.0%) | 8(80.0%) | ||
| Leg pain (VAS) | Preop | 7.3±1.6 | 7.6±2.6 | 6.6±2.6 | 7.3±1.2 | 0.751 |
| Postop a | 2.1±2.3 | 2.3±2.7 | 1.2±1.1 | 2.5±2.8 | 0.661 | |
| Improvement | 5.3±2.7 | 4.7±2.9 | 5.3±2.6 | 4.8±2.0 | 0.922 | |
| Back pain (VAS) | Preop | 8.5±2.2 | 8.7±1.4 | 8±2.1 | 9.1±0.9 | 0.496 |
| Postop a | 2.2±1.3 | 2.7±2.6 | 1.6±1.7 | 2.6±2.8 | 0.686 | |
| Improvement | 6.3±2.3 | 6±2.6 | 6.4±2.2 | 6.5±2.7 | 0.953 | |
| ODI | Preop | 36.7±4.5 | 37.1±5.9 | 32.7±8.2 | 37.1±8.8 | 0.477 |
| Postop | 14.8±4.7 | 15.9±8.8 | 13±8.35 | 15.8±9.3 | 0.908 | |
| Improvement | 21.3±6.9 | 21.2±7.9 | 19.7±10.2 | 21.2±5.0 | 0.984 | |
| Follow-up (m) | 43.1±8.6 | 41.4±9.8 | 35.2±5.3 | 38.5±8.1 | 0.212 | |
aKruskal-Wallis test.
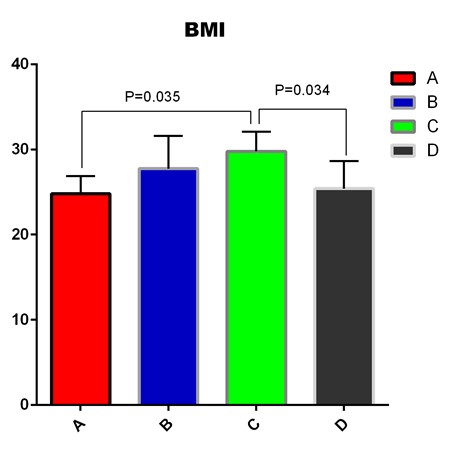
Figure 1. Body Mass Index (BMI) in different types of LDS
To investigate the effect of kyphotic alignment on clinical behavior, we also placed our patients into two groups; kyphotic (type D) and non-kyphotic (types A, B, and C) and compared them with each other (Table 3). Again, we could find no difference.
| Kyphotic group (type D) |
Non-kyphotic group (type A, B, and C) |
P value | ||
| Number |
11(22.4%) | 38(77.6%) | - | |
| Leg pain (VAS) | Preop | 7.3±1.3 | 7.2±2.4 | 0.943 |
| Postop | 2.5±2.8 | 1.9±2.2 | 0.514 | |
| Improvement |
4.8±2.0 | 5.0±2.7 | 0.832 | |
| Back pain (VAS) | Preop | 9.1±1.0 | 8.45±1.7 | 0.252 |
| Postop | 2.6±2.8 | 2.2±22 | 0.701 | |
| Improvement |
6.5±2.7 | 6.2±2.4 | 0.724 | |
| ODI | Preop | 37.0±8.8 | 35.8±6.5 | 0.646 |
| Postop | 15.8±12.3 | 14.9±9.2 | 0.806 | |
| Improvement | 21.2±15.0 | 20.8±8.5 | 0.919 | |
Discussion
One of the issues complicating research on LDS is the lack of a standard to classify the patients into subgroups. There are currently several classification systems for LDS that need further evaluation (5, 7, 11-13). CARDS classification system has been favored due to its ease of use and accuracy. In this study, we tried to examine the outcome of the patients after surgery based on CARDS classification. Generally speaking, this disease is more common in women (2-3:1, female: male) which is related more to hormonal issues and ligamentous laxity (14). Most of the patients in Kung's, Sobol's, and ours were women, but it was only in Chen's study that the number of men was higher (6, 15, 16).
LDS is a disease of old age. Its incidence increases in both sexes with age (1, 14, 17). More than 70% of the patients in our study were middle-aged and older, and type A group had the oldest patients. The mean age of Kung et al.'s study was 62 years old, and type D was the oldest (15).
In the study we carried out, BMI was significantly different across the types and BMI in type C was significantly higher than that in type A and D. The highest BMI in our study was present in type C. The highest BMI in Kung et al.'s and Sobol et al.'s studies were observed in type B and type D, respectively (6, 15), which did not show any significant difference with other types in these two studies. Rihn et al.'s study sought to answer the question of whether obesity affects the outcome of treatment for spondylolisthesis and spinal stenosis (18). They concluded that BMI had no significant effect on the clinical outcome following surgery for lumbar stenosis. Obese patients undergoing surgery experience a higher rate of wound infection, and their reoperation rate is twice higher than non-obese patients in a 4-year follow-up study. Obese patients who did not undergo surgery and were just treated conservatively had worse clinical outcomes than non-obese patients.
In our study, type B had the highest prevalence across different types of LDS and type A had the lowest, while in both Kung et al.'s and Sobol et al.'s studies, type C had the highest and type A had the lowest (6, 15).
Although it was shown that CARDS type D has more segmental instability relative to other types, its relationship with clinical behavior is not clear. It was proposed that in the kyphotic group, the turgor pressure of the disc is reduced due to insufficient support of the anterior column, thereby impairing the disc's ability to withstand anterior shear forces, resulting in a much larger instability (19). In our study, the pain in the leg and back was reduced significantly after surgery, and disability improved significantly by the operation but this improvement in pain and disability did not differ across types of LDS; also, kyphotic alignment had no clinical effect. Contrary to our study, Sobol et al. and Kong et al. in two separate retrospective studies on their operated patients with L4-L5 LDS found that the patients with kyphotic alignment (type D) had worse preoperative back pain and a more favorable response to the surgical treatment in compared with a non-kyphotic group (6, 15). Similar to these two studies, Chen et al. reviewed their patients with LDS operated with transforaminal lumbar interbody fusion and placed them into two groups: kyphotic and non-kyphotic (20). They also found that the patients with kyphotic alignment not only have more dynamic instability and worse preoperative disability and pain but also achieve more clinical improvement with surgical treatment.
This study had several limitations. With a retrospective design and a small sample size, the statistical significance of this study may not guarantee the clinical consequence. The minimum clinically important difference (MCID) is the smallest improvement that is valued by the patient, but this improvement may not be statistically significant in this study. The results of this study were reported using VAS, ODI and no other external criteria were used as dependent variables. We could not obtain a valid MCID due to the lack of a suitable dependent variable. We did not take account of the sagittal balance, which might alter the surgical outcome, although this is not proven for low-grade spondylolisthesis. All of these factors may be biased in this study. Also, our results do not fully represent all patients with spondylolisthesis because only patients referred to one hospital were evaluated. Due to the discrepancy found in our study with similar studies, more research is needed in this area with larger sample size.
Conclusion
In conclusion, surgical treatment of LDS could significantly improve both pain and disability in all different types of the disease, but this improvement was not significantly different across radiographic types. It seems that here, like other areas of the spine, no significant relationship exists between the clinical and radiological characteristics.
Acknowledgements
This study was supported by Students Research Center of Mashhad University of Medical Sciences, Mashhad, Iran. All authors have nothing to declare.
Funding
This work was supported by Students Research Center of Mashhad University of Medical Sciences, Mashhad, Iran [grant NO. 980443].
Conflicts of Interest
The authors declared no potential conflict of interests relevant to this article.
Received: 2021/07/15 | Accepted: 2022/07/4 | Published: 2022/08/8
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |



