BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
URL: http://journal.zums.ac.ir/article-1-7065-en.html


 , Abbas Soltani1
, Abbas Soltani1 

 , Bina Eftekharsadat2
, Bina Eftekharsadat2 

 , Parvin Sarbakhsh3
, Parvin Sarbakhsh3 

 , Mehrdad Habibi1
, Mehrdad Habibi1 

 , Ali E. Oskouei *4
, Ali E. Oskouei *4 


2- Dept. of Physical Medicine and Rehabilitation, Tabriz University of Medical Sciences, Tabriz, Iran
3- Dept. of Epidemiology and Biostatics, Tabriz University of Medical Sciences, Tabriz, Iran
4- Dept. of Physiotherapy, Faculty of Rehabilitation, Tabriz University of Medical Sciences, Tabriz, Iran ,
✅ HPLT combined with the routine physiotherapy improve the clinical as well as sonography findings including supraspinatus tendon thickness and accumulation of sub-acromial fluid in people with rotator cuff tendinitis compared with those in the control group.
Shoulder pain is the main cause of musculoskeletal disorder which usually persists in the middle and older aged people (1). Sub-acromial impingement syndrome, frozen shoulder, shoulder tendinopathy, bursitis, and capsulitis are more common causes of shoulder pain. One of the major causes of shoulder pain is rotator cuff tendinopathy (40%-65%). Rotator cuff muscles including supraspinatus, infraspinatus, subscapularis, and teres minor are stabilizer and mover shoulder muscles (2, 3).
Clinical symptoms of rotator cuff disorders including pain, weakness, and limited shoulder movements especially abduction and rotation mainly lead to impairment in shoulder function, sleep disturbance and quality of life (4, 5). Common treatment of shoulder disorders are as follows: non- steroidal anti-inflammatory drugs (NSAID) (6), corticosteroid injection, and conservative treatment methods including mobilization of the shoulder (7), kinesio taping (8), ultrasound therapy (9), transcutaneous electrical nerve stimulation, shock wave therapy (10), and recently the laser therapy especially high power laser therapy (HPLT) which seems to be a new modality to reduce the inflammation and pain (11, 12).
Laser, an acronym for Light Amplification of Stimulated Emission of Radiation, is categorized as low power and high power lasers. The theory behind the laser therapy is associated with the fact that laser can deeply penetrate the tissue and produce biochemical effects on tissues as well as cell heeling and vascular system stimulation. HPLT has been reported to have some physiological and clinical effects such as reduction of pain, edema, anti-inflammatory role and facilitating the tissue healing, microcirculation, tissue regeneration and early beginning for rehabilitation program. It seems that laser reduces the pain related to inflammation by lowering the levels of prostaglandin E2, interleukin 1-beta, tumor necrosis factor-alpha oxidative stress, and tissue edema (12). The pulse gallium-aluminum-arsenide (Ga-Al-As) laser is a safe, painless, deep penetration modality that is normally used in some musculoskeletal disorders (13, 14). The appropriate dose for anti-inflammatory and pain reduction appears to be between 0.3 and 19.0 J/cm (15).
To the best of our knowledge, the previous studies did not measure the amount of tendon thickness and sub-acromial fluids, as an indication of inflammation, in people with rotator cuff tendinitis. Therefore, the purpose of this study was to investigate the effects of Ga-Al-As HPLT on shoulder pain, passive and active range of motions, functional abilities and sub-acromial liquid and tendon thickness in people with rotator cuff tendinitis. In this study, we assessed the amount of inflammation and fluid accumulation in the sub-acromial region and the thickness of the supraspinatus tendon before and after treatment using sonography.
We hypothesized that HPLT combined with the routine physiotherapy may improve clinical and sonographic findings in rotator cuff tendinitis compared with those in the control group that just received normal and routine physiotherapy.
This study was a randomized clinical trial registered in Iranian Registry of Clinical Trials (IRCT) with the number 20191127045528N1. The patients were recruited from the rehabilitation outpatient clinic. Diagnosis of rotator cuff tendinitis was confirmed by both clinical and sonographic findings. They were then assessed to evaluate their eligibility for the study and to provide detailed information about the study purpose and the treatment protocols. All patients had a restricted shoulder range of motion, pain between 3 to 7 in visual analog scale (VAS), sign of fluid in sub-acromial space confirmed by sonography. The exclusion criteria were a systemic inflammatory disease such as rheumatoid arthritis or osteoarthritis, rotator cuff tears, the humerus fracture, neurological diseases, fibromyalgia syndrome, receiving physiotherapy treatment for this problem at least 6 months before receiving another medicine or injection (12, 13, 16). The sampling period of the study and data collection took place between January 2020 and October 2020.
The patients were informed of the study purpose and the treatment methods. Written informed consent was then obtained from all of the subjects, and the protocol was approved by the Ethics Committee of Tabriz University of Medical Sciences (IR.TBZMED.REC.1398.837). The total number of 32 patients ranging from 40 to 60 years-old participated in this study. They were then randomly assigned to the control group (n=16) that received routine physiotherapy including TENS (Model 710 P, Novin Company), Ultrasound) Model 215 M, Novin Company), hot pack, exercise consisting range of motion, pendulum, strengthening, and stability exercises, or the treatment group (n=16) that received routine physiotherapy and HPLT (Model 885 G, Novin Company).
For the control and treatment groups, TENS along with hot pack was applied to the anterior and posterior aspects of the shoulder for 20 minutes each session, 3 days a week (12 sessions), at a frequency of 100 Hz, with a pulse duration of 50 μs, and at an intensity with a comfortable tingling sensation. Therapeutic ultrasound was then applied to the tendonitis area for 5 minutes per session, at a frequency of 3 MHz, with an intensity of 1 W/cm2 and a duty cycle of 50%.
Following the routine physiotherapy modalities, patients in the control group performed the regular exercises including the range of motion exercises with the purpose of increasing shoulder flexion, abduction, internal and external rotation, pendulum exercises, rotator cuff isometric exercise in pain free range of motion 3 days a week and 10 repetitions of each exercise. The placebo laser was also applied to the shoulder area in the control group. The treatment group was identical to the control group, except that Ga-Al-As HPLT was applied in 10 tender points around the shoulder joint (each pain area for 20s, totally 200s) per session in a position of shoulder internal rotation, with an average power of 4w, wavelength of 808nm, energy density of 20J/cm2, and with spacer of 2.5cm to avoid any possible and thermal damage (Table 1). Pain was assessed from 0 to 10 by visual analogue scale (17) which indicated no pain and maximum pain, respectively before and after 12 treatment sessions.
Passive and active shoulder range of motion consisting abduction, forward flexion, external and internal rotation were assessed before and after 12 treatment sessions with goniometer approach. The goniometry was approved at greater tubercle for forward flexion, acromion for abduction, and olecranon for internal and external rotation at 45 degrees shoulder abduction and 90 degrees elbow flexion (18). All patients were also assessed before and after study by a reliable and validated shoulder pain and disability index (SPADI), consisting of two parts. The first part of the SPAID consists of 5 items related to pain and the second part consists of 8 items related to the ability of the shoulder. The scores are from 0 to 10, which indicated no pain or disability and maximum pain or disability, respectively (19).
Sonography approach
Accumulation of the sub-acromial fluid before being referred to the current study was assessed by a specialist using Samsung's ultrasonic device model WS80A with a frequency of 13MHz. The amount of sub-acromial fluid accumulation and tendon thickness (from the articular margin) were measured while the patients were sitting with their hands on the buttocks and internal rotation of the shoulder (Figure 1), in the longitudinal axis of the tendon and sagittal ablation (20).
 |
 |
Figure 1. Patient's position and sonography device.
Table 1. High power laser features
| W8 4w 2.5 Cm 20Hz 808nm 200s 800j 10 tender points 3 session per 4 weeks |
Peak power Average power Probe spacer Frequency Wavelength Total time treatment Total energy Treatment approach Treatment sessions |
Statistical analysis
Statistical analysis was performed by using Statistical Package for Social Sciences, version16.0 SPSS, Chicago, IL, USA). The mean, the standard errors and the percentage of improvement in outcome measures were measured for all participants in the control and treatment groups. Wilcoxon test and Mann-Whitney U test were used for within-group and between-group comparisons, respectively. Significance was accepted for values of p<0.05 in all analyses.
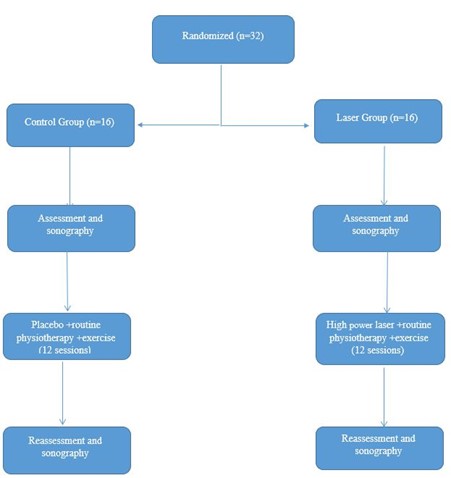
Figure 2. Flow diagram of the study
Figure 2 presents the complete research. Flow diagram of the study. A total of 32 patients (control group: 10 males and 6 females; treatment group: 7 males and 9 females) with the mean age of 46±8.53 years in the treatment group and 39±8.68 years in the control group with rotator cuff tendinitis were studied Clinical and sonography characteristics of the patients consisting passive and active shoulder abduction, forward flexion, external and internal rotation, as well as pain and disability index using SPADI, amount of sub-acromial fluid accumulation and tendon thickness are presented in Table 2. There were no statistically significant between-group differences in any clinical characteristics of the study patients with rotator cuff tendinitis before treatment except sub-acromial liquid (Table 2, P>0.05).
All clinical characteristics and sonography findings except rotator cuff thickness were improved after treatment in both groups (Table 2, P<0.05).
Table 2. Outcome variable of both groups
| Outcome variable | HPLT Group (n = 16) |
Control Group (n = 16) | P |
| Active shoulder abduction | |||
| Baseline | 91.50±27.16 | 82.00±23.75 | 0.59 |
| Post treatment | 119.56±23.09 | 87.68±23.95 | 0.001 |
| p-value | 0.001 | 0.001 | |
| Passive shoulder abduction | |||
| Baseline | 97.75±26.51 | 86.75±23.62 | 0.49 |
| Post treatment | 129.62±19.56 | 91.75±24.65 | 0.001 |
| p-value | 0.001 | 0.004 | |
| Active shoulder flexion | |||
| Baseline | 99.93±26.62 | 90.12±17.08 | 0.18 |
| Post treatment | 133.5±20.33 | 96.37±17.22 | 0.001 |
| p-value | 0.001 | 0.001 | |
| Passive shoulder flexion | |||
| Baseline | 111.75±25.09 | 95.43±16.79 | 0.07 |
| Post treatment | 141.31±20.64 | 102.31±17.83 | 0.001 |
| p-value | 0.001 | 0.001 | |
| Active shoulder external rotation | |||
| Baseline | 54.43±14.06 | 57.87±17.86 | 0.61 |
| Post treatment | 65.42±11.93 | 62.93±15.71 | 0.61 |
| p-value | 0.001 | 0.001 | |
| Passive shoulder external rotation | |||
| Baseline | 58.31±14.32 | 59.37±18.40 | 0.89 |
| Post treatment | 70.06±11.20 | 64.87±16.82 | 0.36 |
| p-value | 0.001 | 0.001 | |
| Active shoulder internal rotation | |||
| Baseline | 47.12±13.25 | 47.00±6.82 | 0.8 |
| Post treatment | 53.25±7.63 | 52.56±6.08 | 0.69 |
| p-value | 0.007 | 0.001 | |
| Passive shoulder internal rotation | |||
| Baseline | 48.06±6.69 | 50.00±8.52 | 0.51 |
| Post treatment | 57.25±5.98 | 54.62±10.17 | 0.34 |
| p-value | 0.001 | 0.01 |
| Outcome variable | HPLT Group (n = 16) |
Control Group (n = 16) |
P |
| VAS | |||
| Baseline | 7.31±1.40 | 6.81±1.32 | 0.28 |
| Post treatment | 2.62±0.8 | 5.18±1.32 | 0.001 |
| p-value | 0.001 | 0.001 | |
| SPADI (pain) | |||
| Baseline | 38.06±4.31 | 35.87±8.82 | 0.98 |
| Post treatment | 15.57±4.02 | 29.56±9.15 | 0.001 |
| p-value | 0.001 | ||
| SPADI(disability) | |||
| Baseline | 55.68±6.92 | 53.50±6.84 | 0.53 |
| Post treatment | 23.31±5.64 | 43.68±9.19 | 0.001 |
| p-value | 0.001 | 0.001 | |
| Subacromial liquid | |||
| Baseline | 2.22±0.44 | 1.60±0.37 | 0.001 |
| Post treatment | 0.68±0.38 | 1.28±0.36 | 0.001 |
| p-value | 0.001 | 0.001 | |
| Tendon thickness | |||
| Baseline | 6.01±0.71 | 6.02±0.69 | 127.50 |
| Post treatment | 5.56±0.49 | 5.79±0.63 | 0.22 |
| p-value | 0.001 | 0.001 |
(HPLT: high power laser therapy, VAS: visual analogue scale, SPADI: shoulder pain and disability index).
There was no difference in the thickness of the rotator cuff muscle tendon, especially the supraspinatus muscle tendon before and after the intervention, and the normal thickness of the supraspinatus tendon was 5 mm according to previous studies.
Discussion
The aim of this study was to evaluate the effect of high-intensity laser Ga-Al-As along with exercise therapy on pain, shoulder range of motion, shoulder disability and sub-acromial fluid accumulation and tendon thickness. Various modalities are used to reduce the symptoms of sub-acromial impingement syndrome. Low level laser is highly recommended for reducing pain but in some studies it has not been reported to be very effective in increasing range of motion, so to improve shoulder function and range of motion, Exercise therapy is recommended (21).
The results of our present study showed that high power lasers can significantly improve pain, shoulder joint function, range of motion, and reduction of sub-acromial fluid but do not affect tendon thickness after treatment.
Laser can reduce the symptoms related to pain and inflammation of frozen shoulder (22), ankle pain (12), knee osteoarthritis (23), back pain (24) In general, lasers can affect cellular and tissue activity and on the other m RNA hand increase mitochondrial aerobic activity and increase the production of ATP. The analgesic and anti-inflammatory effects of lasers can be effective in treating musculoskeletal disorders (25). The soothing effects of high-intensity lasers can be related to delays in the transmission of pain messages along pain-related nerve fibers, as well as an increase in encephalin and endorphins. In addition, the laser has a direct effect on nerve structures and accelerates the rate of nerve recovery and increases blood circulation, thereby helping to guide the nerve (26).
Our study showed that the combined effects of HPLT with exercise therapy are more effective than placebo laser and exercise therapy. The findings of Santamato et al. are consistent with our study, which shows the effectiveness of HPLT in reducing pain, disability and inflammation in patients with sub-acromial impingement syndrome (16).
Out study also supports some studies in which low-power lasers had positive effect of reducing pain (27, 28). In contrast, the study by Kim et al did not prove the effect of high power lasers in reducing pain (29). Sebnem Koldas Dogan et al showed that low-intensity lasers combined with exercise therapy and cold therapy have no effects on pain of shoulder joint disorders (30).
Although the parameters used in the high- intensity laser in this study in terms of wavelength, energy density, intensity, and penetration are different from the low- intensity laser used in previous studies, these differences may explain the conflicting findings of the current study.
Four weeks of therapeutic exercise program to increase range of motion, muscle strength, and flexibility of the posterior shoulder capsule may also reduce pain and improve function in these patients.
In recent years, high-intensity laser has been widely used in the treatment of neuromuscular conditions, and this modality is able to deeply stimulate the joints and muscles. Maybe, high- intensity lasers can reduce pain and improve performance compared with low intensity lasers. The discrepancies reported between these studies may be due to different patient selection criteria and parameters used in laser therapy and measurement criteria.
Conclusion
From the results of this study, we concluded that high power laser therapy in combination with the routine physiotherapy improve the clinical (pain, range of motion, function and sub- acromial liquid reduction) as well as sonography findings including supraspinatus tendon thickness and accumulation of sub-acromial fluid in people with rotator cuff tendinitis. These findings might be associated with decrease in inflammation by lowering the levels of PGE2 and some other factors in cell culture.
Study limitation
In our study the follow-up period was relatively short for understanding the maintenance of the long-term effects of HPLT in patients with rotator cuff tendonitis.
Acknowledgements
The authors would like to thank the Tabriz University of Medical Sciences for providing the setting to perform this study.
Funding
This study was funded by the Tabriz University of Medical Sciences.
Authors' contributions
M. B.: Conceptualization, data collection, writing first draft. A. S.: Conceptualization, methodology. B. E.: Data collection, sonography. P. S.: Statistical analysis. M. H.: Data collection, data analysis. A. E O.: Conceptualization, methodology, supervision, writing and editing final draft and project administration.
Conflicts of Interest
There is no financial and personal relationship with other people or organizations that could inappropriately influence this work.
Received: 2023/06/24 | Accepted: 2023/09/9 | Published: 2024/01/29
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |