BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
URL: http://journal.zums.ac.ir/article-1-6735-en.html


 , Zahra Bahari2
, Zahra Bahari2 

 , Shahin Zekriamir1
, Shahin Zekriamir1 

 , Hassan Shahriary1
, Hassan Shahriary1 

 , Mohammad Javad Behzadnia *3
, Mohammad Javad Behzadnia *3 


2- Dept. of Physiology and Medical Physics, Faculty of Medicine, Baqiyatallah University of Medical Sciences, Tehran, Iran
3- Trauma Research Center, Baqiyatallah University of Medical Sciences, Tehran, Iran ,
✅The present study suggested that CABG and CHF had a significant relationship with unsuccessful resuscitation. Furthermore, cardiomyopathy, CABG, renal disease, and poisoning were significantly associated with mortality.
Cardiac arrest (CA) is the most common cause of death with poor prognosis, and remains a major public health burden globally (1). CA is characterized as the sudden cessation of spontaneous cardiac mechanical activity, pulmonary ventilation, and circulating blood flow (2). Based on where they occurr, CAs are divided into two types, including out-of-hospital arrests and in-hospital arrests. It is reported that the mortality rate is higher in out-of-hospital arrests than in-hospital arrests (1). Cardiopulmonary resuscitation (CPR) is an attempt to restore cardiac electrical and mechanical activity via various interventions, including early pharmacological interventions, airway interventions, and chest compressions (2, 3). However, survival with good quality of life is rare following CA (3). Hence, clarifying the predictors of CA survival could improve decision making for clinicians when considering the appropriate application of CPR interventions (3). Furthermore, it is critical that patients with poor chance of survival receive high quality care (4). Today, the association between pre-CA comorbidity and the CA outcome in different populations is still unclear. For example, Hirlekar et al., (2018) reported that the most common comorbidities in patients with CA were a history of congestive heart failure (CHF), myocardial infarction, and diabetes (4). It has been established that patient comorbidity can affect the outcome after CA. Therefore, identifying the risk factors of CA is imperative. Several investigations revealed that pre-CA comorbidity is related to complications following CA with higher mortality rates (5-8). For instance, Andrew et al., evaluated the effect of the Charlson Comorbidity Index (CCI) on survival to hospital discharge of patients with out-of-hospital CA. They reported that reduced odds of survival were associated with increased CCI (1). However, there are conflicting studies in this area. For example, in a prospective study, Beesems et al., found that there was no effective association between pre-history comorbidity and the survival/neurological outcome in older patients with out-of-hospital CA (9). Therefore, to date, the effects of pre-CA comorbidities on the outcomes have not been fully understood (1). The aim of the present study was to investigate the association of pre-existing comorbidity with the mortality rate and unsuccessful CPR (worse outcomes) in all the CA patients (1320 patients) who were admitted to Baqiyatallah Hospital (Tehran, Iran), and underwent CPR from 2018 to 2020. We also evaluated the association of demographic data (gender and age) with mortality and unsuccessful CPR.
Ethical considerations
The current retrospective study was approved by the Research Ethics Committee, Hospital (Tehran, Iran) (Ethical code: IR.BMSU.REC.1399.009).
Data collection
Data of all the admitted CA patients, who underwent CPR [according to the standard method of resuscitation (11)] from 2018 to 2020 were retrospectively reviewed. We extracted the demographic data (age and gender), as well as information regarding the location of CA, causes of CPR, comorbidities, and frequency of mortality and unsuccessful CPR. Additionally, we analyzed the association of comorbidity data with mortality and unsuccessful CPR. We also investigated the relationship of the demographic data (gender and age) with mortality and unsuccessful CPR.
Statistical analysis
The present data were analyzed using SPSS software (version 16.0). Qualitative variables were evaluated using Pearson's chi-square test. Quantitative variables were examined using Pearson's regression. For the quantitative variable (age), data are presented as mean ± standard error of the mean (SEM). For qualitative variables data are presented as frequency and percentage. In the present study, a p-value of 0.05 or lower is considered statistically significant.
Demographic characteristics of patients
A total of 1320 patients were included in the present study, from 2018 to 2020 (study period: two years). The average duration of CPR in all the patients was 34.18 ± 0.38 min (the minimum duration was 30 min and the maximum duration was 210 min). CPR was performed at least once and a maximum of four times for patients. The mean age of all the patients was 65.60 ± 0.426 (mean± SEM) years (minimum=1 years and maximum=108 years). Most of the patients were in the age group of 70 to 79 years (N=330). In the present study, 794 (60.2%) patients were men, 517 (39.2%) patients were women, and 9 (0.7%) had missing data (total=1320). Most CAs occurred in hospital (1289), of these, 782 of patients were men and 507 of patients were women. Of the 1320 patients, 923 died and 396 patients survived (Figure 1, missing data=1). The case fatality rate (CFR) of CA was 69.92%.
Figure 1. The mortality rate of all patients. (A) The frequency of patients’ mortality (missing data=1); (B) the frequency of patients based on gender× mortality following CA (cross tabulation, missing data=9).
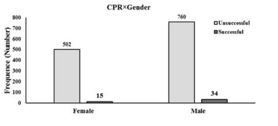
Of the 1320 patients, CPR was unsuccessful in 1271 (96.3%). Of 1271 patients with unsuccessful CPR, 502 patients were female and 760 s were male (Figure 2).
Figure 2. The frequency of patients based on gender× successful CPR following CA (cross tabulation, missing data=9).
Association between demographic data (gender and age) and mortality/ unsuccessful CPR
Our data analysis (using the chi-square test) revealed that gender (odds ratio [OR] 0.913; 95% CI 0.717‒1.161, P-value=0.458) had no significant relationship with mortality. Similarly, gender (OR: 0.668, 95% CI 0.360‒1.239, P-value=0.198) showed no significant relationship with the unsuccessful CPR. Furthermore, our data analysis (using Pearson Regression) revealed that age (R = 0.64, R square =0.004, P-value=0.023) was significantly associated with the mortality, however, age (R=0.026, R square=0.001, P-value=0.354) had no significant association with unsuccessful CPR.
Association between causes of CPR and mortality
According to our results, CA (903, 68.4%), respiratory arrest (506, 38.3%), impaired consciousness (283, 21.4%), respiratory distress (244, 18.5%), and arrhythmia (195, 14.8%) were the main causes of CPR in the patients (Table 1). It was found that CA (OR 4.170; 95% CI 3.24‒5.26, P-value=0.000), respiratory distress (OR 0.25; 95% CI 0.19‒0.34, P-value=0.000), and impaired consciousness (OR 0.35; 95% CI 0.27‒0.47, P-value=0.000) were significantly associated with mortality (Table 1).
Table 1. The primary causes of CPR in all patients (1320)
| Cause of CA | Frequency (%) | Mortality (N) | P-Value |
| Arrhythmia | 195 (14.8%) | 142 | 0.348 |
| Cardiac Arrest | 903 (68.4%) | 720 | 0.000 |
| Respiratory Arrest | 506 (38.3%) | 369 | 0.054 |
| Respiratory Distress | 244 (18.5%) | 108 | 0.000 |
| Impaired Consciousness | 283 (21.4%) | 146 | 0.000 |
| Others | 7 (0.5 %) | 4 | 0.458 |
The data are presented as numbers and percentages (%). The P-values demonstrated a statistically significant association between the primary causes of CPR and mortality.
Association between comorbidities and mortality
In the current study, we assessed 11 common comorbidities in all the patients. Our analysis showed that the most common comorbidities were cancer (28.9%), respiratory disease (14.3%), and renal disease (10.4%) (Table 2). Cardiomyopathy (OR 0.371; 95% CI 0.133‒1.029, P-value=0.048), coronary artery bypass grafting (CABG) (OR: 0.421, 95% CI 0.193‒0.916, P-value=0.025), renal disease (OR 0.671; 95% CI 0.465‒0.969, P-value=0.032), and poisoning (OR 0.142; 95% CI 0.15‒1.370, P-value=0.049) were significantly associated with mortality (Table 2).
Table 2. The association of comorbidities with mortality and unsuccessful CPR.
| Comorbidities-Frequency (total patients:1320) |
Frequency | Mortality | Successful CPR | P-Value Comorbid×mortality |
P-Value Comorbid×CPR |
|
Heart-related disease
Cerebrovascular arrest
Hypertension Diabetes mellitus Respiratory disease Renal disease Liver disease Electrolyte disorder Cancer Poisoning Sepsis |
15 (1.1%) 7 (0.5%) 26 (2.0%) 65 (4.9%) 45 (3.4%) 67 (5.1%) 42 (3.2%) 62 (4.7%) 189 (14.3%) 137 (10.4%) 38 (2.9%) 5 (0.4%) 382 (28.9%) 4 (0.3%) 122 (9.2%) |
7 3 13 41 27 50 24 41 121 85 26 3 277 1 89 |
1 1 5 7 2 1 2 2 4 7 1 0 10 0 1 |
0.048 0.117 0.025 0.213 0.137 0.394 0.065 0.498 0.054 0.032 0.832 0.626 0.200 0.049 0.460 |
0.543 0.138 0.000 0.002 0.791 0.324 0.715 0.836 0.210 0.361 0.721 0.660 0.180 0.694 0.076 |
CABG: coronary artery bypass grafting, CHF: congestive heart failure, AMI: acute myocardial infarction.
Association between comorbidities and unsuccessful CPR
Present data revealed that CABG (OR 6.764; 95% CI 2.438‒18.769, P-value=0.000), and CHF (OR 3.486; 95% CI 1.501‒8.093, P-value=0.002), were significantly associated with the unsuccessful CPR (Table 2).
Discussion
Direct laryngoscopy is usually associated with hemodynamic stress responses which in turn increases the risk of perioperative myocardial ischemia espe-cially in CABG [12-15]. According to the results of the current study, lower doses of esmolol infusion prevent the elevation of
Conclusion
According to the results of the current study, the applied doses of esmolol infusion significantly reduced SBP during intubation. Hemodynamic changes were significant over time; in addition, SBP, MAP, and HR changes were not significant in the infusion group, compared with the
Acknowledgements
The manuscript was part of a research project approved by Kashan University of Medical Sciences and the local ethical committee (Code No. ir.Kaums.rec.1394.19; date: 24 May, 2015).
Conflicts of Interest
None.
Received: 2021/09/28 | Accepted: 2022/07/26 | Published: 2022/12/12
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |